CANNABIS AS AN EXIT DRUG
As part of its official religion, alcohol
has been protected in Slovenia, and users wishing to transition to a safer drug
have been told the cure is illegal and immoral or something, stigmatised,
criminalised, and used as a cash cow by the judiciary, in the way alcoholics
tend to see the economy.
Typically, Slovenia has not noticed
anything non-economic about cannabis. To Slovenia, a suicide is not a wasted
life, but a waste of educational resources. But it has been observed that
alcohol and cannabis are substitutes when it comes to user expenditure.
https://www.tandfonline.com/doi/full/10.1080/1331677X.2018.1561321 [806]
"L'alcoolisme a conduit 2 membres de
ma famille au suicide. Le cannabis a permis à 2 autres d'arrêter l'alcool."
https://twitter.com/ConradMaj [808]
According to Tod H Mikuriya (2004):
"No clinical trials of the efficacy of cannabis as a substitute for alcohol are
reported in the literature, and there are no papers directly on point prior to
my own account (Mikuriya 1970) of a patient who used cannabis consciously and
successfully to discontinue her problematic drinking. There are ample
references, however, to the use of cannabis as a substitute for opiates (Birch
1889) and as a treatment for delirium tremens (Clendinning 1843; Moreau 1845),
which were among the first uses by European physicians. The 1873 Indian
Government Finance Department Resolution recommended against suppressing
cannabis use for fear that people (p. 1395) 'would in all probability have
recourse to some other stimulant such as alcohol.'
"The Indian Hemp Drugs Commission Report of (1893-1894) articulated the same
concern (p. 359): '. . . driving the consumers to have recourse to other
stimulants or narcotics which may be more deleterious.
"Birch (1889) described a patient weaned off alcohol by use of opiates who then
became addicted and was weaned off opiates by use of cannabis. He noted (p.
625), 'Ability to take food returned. He began to sleep well; his pulse
exhibited some volume; and after three weeks he was able to take a turn on the
verandah with the aid of a stick. After six weeks he spoke of returning to his
post, and I never saw him again.'"
Reviewing his own 92 patients using cannabis as an alcohol substitute:
"All patients reported benefit, indicating that for at least a subset of
alcoholics, cannabis use is associated with reduced drinking."
https://hams.cc/mikuriya.pdf [3822]
In "Reductions in alcohol use following medical cannabis initiation: results
from a large cross-sectional survey of medical cannabis patients in Canada",
Lucas et al (2020) found the same, rather obvious, thing, publishing their
results almost 21 years after the ZPPPD in the International Journal of Drug
Policy:
"Background: Evidence details how
cannabis can influence the use of other psychoactive substances, including
prescription medications, alcohol, tobacco and illicit drugs, but very little
research has examined the factors associated with these changes in substance use
patterns. This paper explores the self-reported use of cannabis as a substitute
for alcohol among a Canadian medical cannabis patient population.
"Methods: Data was derived from a
survey of 2102 people enrolled in the Canadian medical cannabis program. We
included 973 (44%) respondents who reported using alcohol on at least 10
occasions over a 12 month period prior to initiating medical cannabis, and then
used retrospective data on the frequency and amount of alcohol use pre-and post
medical cannabis initiation to determine which participant characteristics and
other variables were associated with reductions and/or cessation of alcohol use.
"Results: Overall, 419 (44%)
participants reported decreases in alcohol usage frequency over 30 days, 323
(34%) decreased the number of standard drinks they had per week, and 76 (8%)
reported no alcohol use at all in the 30 days prior to the survey. Being below
55 years of age and reporting higher rates of alcohol use in the pre-period were
both associated with greater odds of reducing alcohol use, and an intention to
use medical cannabis to reduce alcohol consumption was associated with
significantly greater odds of both reducing and ceasing alcohol use altogether.
"Conclusions: Our findings suggest
that medical cannabis initiation may be associated with self-reported reductions
and cessation of alcohol use among medical cannabis patients. Since alcohol is
the most prevalent recreational substance in North America, and its use results
in significant rates of criminality, morbidity and mortality, these findings may
result in improved health outcomes for medical cannabis patients, as well as
overall improvements in public health and safety."
https://www.sciencedirect.com/science/article/abs/pii/S0955395920303017?via%3Dihub
[399]
Pince et al (2025) found similar support for substitution:
"We investigated the effects of legal-market cannabis on alcohol
self-administration and craving using a within-subjects human laboratory drug
administration paradigm. We tested whether cannabis serves as a substitute for
alcohol (i.e., attenuating alcohol consumption and craving) in a sample of
community adults who drink heavily and use cannabis regularly. Consistent with
our hypothesis, we found that across the entire sample, self-administering
cannabis before alcohol significantly reduced alcohol consumption compared to
when alcohol was offered without cannabis. Furthermore, we found that cannabis
and alcohol co-administration was associated with significant acute reduction in
alcohol craving compared to alcohol administration alone."
In "the first study to test effects of legal-market cannabis on alcohol
intake...Cannabis use was associated with a reduction in alcohol intake...Those
who drank less after cannabis reported greater decreases in alcohol craving"
reported Pince et al (2025):
"While human laboratory studies are comparatively limited, Mello and colleagues
instructed participants to complete a basic operant task wherein they could earn
cannabis or money after 30 min of work and alcohol after 15 min, and found that
individuals self-administered less alcohol when cannabis was concurrently
available (Mello et al., 1978). Later, Ballard and DeWitt found that
co-administration of low doses of THC and alcohol reduced alcohol craving
(Ballard and de Wit, 2011). An unpublished laboratory study also observed that
cannabis use was associated with acute reductions in alcohol intake and some
measures of craving in a within-subjects design with individuals who engage in
heavy drinking (Metrik et al., unpublished). Other observational studies have
reported similar reductions in alcohol consumption when cannabis was used before
alcohol (Gunn et al., 2021; Karoly et al., 2023, Karoly et al., 2024; Rootman,
2020). The effects of cannabis on alcohol craving and consumption during
simultaneous use may be mediated in part by subjective effects (i.e., relaxation
versus stimulation), as simultaneous use predicted discontinuation of drinking
via increased relaxation and decreased alcohol craving at the event-level in an
ecological momentary assessment study (Waddell et al., 2024). Together, these
findings suggest the potential for cannabis to act as a substitute for alcohol.
Further research is needed to elucidate variables that may predict such
substitution behavior."
https://www.sciencedirect.com/science/article/abs/pii/S0376871625003138
[4933]
Gunn et al (2025) think "Working memory
capacity predicts cannabis-induced effects on alcohol urge":
"Participants aged 21 to 44 (N = 125, 32 % female) reporting heavy alcohol use
and cannabis use ≥ twice weekly completed a laboratory protocol across three
days where they smoked a placebo, 3.1 % delta-9 tetrahydrocannabinol (THC), and
7.2 % THC cannabis cigarette. Participants were asked to rate their alcohol urge
pre and post smoking. Prior to the experimental sessions, participants completed
WMC measures including the n-back and the complex span tasks, operation span
(OS) and symmetry span (SS).
"Results
Those with higher WMC, as assessed via the SS task, reported significantly lower
alcohol urge after smoking the 7.2 %, but not the 3.1 %, THC dose, relative to
placebo. Performance on the OS task was not associated with alcohol urge. Lower
WMC as determined via n-back scores was associated with higher alcohol urge
overall, but n-back scores did not moderate the impact of cannabis on alcohol
urge.
"Conclusion
Findings suggest individuals with higher but not lower working memory experience
lower alcohol urge under acute effects of cannabis. Although cannabis is
increasingly perceived as a substitute for alcohol, individuals with lower
working memory may be less likely to experience such benefits when attempting to
reduce their drinking."
https://www.sciencedirect.com/science/article/pii/S030646032500334X?via%3Dihub
[5664]
In "Acute cannabidiol administration reduces alcohol craving and cue-induced
nucleus accumbens activation in individuals with alcohol use disorder: the
double-blind randomized controlled ICONIC trial" and using CBD only, Zimmermann
et al (2024) were able to confirm the effect of cannabis on craving found in
alcoholism and addiction in general [see
2978].
"Here we report data from the double-blind randomized controlled ICONIC trial
that compared the effects of a single dose of 800 mg cannabidiol against placebo
(PLC) in N = 28 individuals with AUD. Cue-induced nucleus accumbens (NAc)
activation, alcohol craving during a combined stress- and alcohol cue exposure
session, as well as craving during an fMRI alcohol cue-reactivity task and CBD
plasma levels served as outcomes. Individuals receiving CBD showed lower
bilateral cue-induced NAc activation (tleft_NAc(23) = 4.906, p < 0.001,
d = 1.15; tright_NAc (23) = 4.873, p < 0.001, d = 1.13) and reported
significantly lower alcohol craving after a combined stress- and alcohol cue
exposure session (Fgroup(1,26) = 4.516, p = 0.043, eta2 = 0.15) and during the
fMRI cue-reactivity task (Fgroup(1,24) = 6.665, p = 0.015, eta2 = 0.23). CBD
levels were significantly higher in the CBD group (t(25) = 3.808, p < 0.001,
d = 1.47) and showed a significant negative association with alcohol craving
during the cue exposure experiment (r = −0.394, pFDR = 0.030) and during fMRI
(r = −0.389, pFDR = 0.030), and with left and right NAc activation
(rleft_NAc = −0.459, pFDR = 0.030; rright_NAc = −0.405, pFDR = 0.030). CBD’s
capacity to reduce stress- and cue-induced alcohol craving and to normalize NAc
activation – a region critical to the pathophysiology of AUD – contribute to
understanding the neurobiological basis of its clinical effects and support its
potential as a treatment option for AUD."
https://www.nature.com/articles/s41380-024-02869-y [3787]
CBD was an exit drug for fruit flies in
"Long term exposure to dietary cannabinoids inhibits rapid functional tolerance
to ethanol in Drosophila melanogaster adults" by Vidal et al (2025):
"Given that CBD acts as a natural antagonist of CB1R, and CB1R antagonists have
been shown to reduce the self-administration and appetitive value of ethanol in
rodent models (Arnone et al., 1997; Economidou et al., 2006), as well as inhibit
the development of rapid tolerance to ethanol in rats (Lemos et al., 2007), CBD
had long been viewed as a promising pharmacotherapy candidate to treat alcohol
used disorders (AUD). Accordingly, CBD treatment was shown to inhibit the
context-dependent relapse into alcohol seeking in rats with a history of alcohol
consumption (Gonzalez-Cuevas et al., 2018), and their ability to develop
tolerance to sedation by alcohol following re-exposure (Szulc et al., 2023). Not
surprisingly, most previous work has focused on the potential role of
CB1/2R-dependent signaling in the cross-talk between ethanol and CBD. Notably,
Viudez-Martinez and colleagues showed that a 5HT1A serotonin receptor antagonist
could block the reduction in alcohol self-administration triggered by the
combined treatment with CBD and naltrexone (Viudez-Martínez et al., 2018),
establishing a precedent for the potential involvement of non-canonical
cannabinoid signaling in the cross-talk between CBD and alcohol."
https://www.micropublication.org/journals/biology/micropub-biology-001825
[5816]
In a prelude to their larger 2021
study "Cannabis Significantly Reduces the Use of Prescription Opioids and
Improves Quality of Life" [2815] in 2017 Lucas and Walsh published a study in
which they surveyed 271 medical cannabis patients in research funded by Tilray.
"Findings include high self-reported
use of cannabis as a substitute for prescription drugs (63%), particularly
pharmaceutical opioids (30%), benzodiazepines (16%), and antidepressants (12%).
Patients also reported substituting cannabis for alcohol (25%),
cigarettes/tobacco (12%), and illicit drugs (3%). A significant percentage of
patients (42%) reported accessing cannabis from illegal/unregulated sources in
addition to access via LPs, and over half (55%) were charged to receive a
medical recommendation to use cannabis, with nearly 25% paying $300 or more."
https://www.sciencedirect.com/science/article/abs/pii/S0955395917300130
[3083]
Holman et al
"...conducted an anonymous,
cross-sectional online survey in May 2021 for seven days with adult Canadian
federally-authorized medical cannabis patients (N = 2697) registered with two
global cannabis companies to evaluate patient perceptions of Primary Care
Provider (PCP) knowledge of medical cannabis and communication regarding medical
cannabis with PCPs, including PCP authorization of licensure and substitution of
cannabis for other medications. … Overall, 47.1% of participants reported
substituting cannabis for pharmaceuticals or other substances (e.g., alcohol,
tobacco/nicotine).”
https://jcannabisresearch.biomedcentral.com/counter/pdf/10.1186/s42238-022-00141-0.pdf
[1826]
Similar results for alcohol came from
Kruger et al (2026) at Buffalo University, NY, for whom cannabis is a "novel
harm reduction strategy":
"Alcohol consumption is associated with nearly 200 health conditions. As
cannabis-infused beverages emerge in the legal market, their potential as a
substitute for alcohol is of growing interest. This study investigates whether
cannabis beverages may reduce alcohol use.A total of 438 anonymous adults who
used cannabis in the past year completed a survey including cannabis use and
alcohol consumption items from the Behavioral Risk Factor Surveillance System
(BRFSS). Chi-square and t-tests compared alcohol use between cannabis beverage
users and non-users, and before vs. after cannabis beverage initiation.About
one-third (33.6%) of respondents used cannabis beverages, typically consuming
one per session. Users were more likely to report substituting cannabis for
alcohol (58.6%) than non-users (47.2%). They also reported fewer weekly
alcoholic drinks after starting cannabis beverages (M = 3.35) compared to before
(M = 7.02), and binge drank less frequently (80.7% reported less than monthly or
never, vs. 47.2% before). Those who cited reducing other substance use were more
likely to use cannabis beverages (45.8%).Findings suggest cannabis beverages may
support alcohol substitution and reduce alcohol-related harms, offering a
promising alternative for individuals seeking to lower alcohol intake."
https://pubmed.ncbi.nlm.nih.gov/41533430/ [5873]
Anderson et al at the National Bureau
of Economic Research:
"...find that both state MMLs and
RMLs are associated with decreases in teen marijuana consumption, consistent
with the hypothesis that selling to minors becomes a relatively risky
proposition for licensed marijuana dispensaries. In addition, we find that MMLs
are associated with decreases in teen cigarette use."
https://www.nber.org/system/files/working_papers/w26780/w26780.pdf [400]
Raman and Bradford (2022) find
"Recreational cannabis legalizations associated with reductions in prescription
drug utilization among Medicaid enrollees":
"We use quarterly data for all
Medicaid prescriptions from 2011 to 2019 to investigate the effect of
state-level RCLs [recreational cannabis laws] on prescription drug utilization.
We estimate this effect with a series of two-way fixed effects event study
models. We find significant reductions in the volume of prescriptions within the
drug classes that align with the medical indications for pain, depression,
anxiety, sleep, psychosis, and seizures. Our results suggest substitution away
from prescription drugs and potential cost savings for state Medicaid programs.”
https://onlinelibrary.wiley.com/doi/10.1002/hec.4519 [1827]
In Canada, Jeddi et al examined "Cost-Effectiveness of Medical Cannabis Versus
Opioids for Chronic Noncancer Pain" (in Canadian dollars):
"Total mean annual cost per patient was $1,980 for oral medical cannabis and
$1,851 for opioids, a difference of $129 (95% confidence interval [CI]: -$723 to
$525). Mean QALYs were 0.582 for both oral medical cannabis and opioids (95% CI:
-0.007 to 0.015). Cost-effectiveness acceptability curves showed that oral
medical cannabis was cost-effective in 31% of iterations at willingness-to-pay
thresholds up to $50,000/QALY gained. Use of opioids is associated with nonfatal
and fatal overdose, whereas medical cannabis is not. Discussion: Our findings
suggest that medical cannabis as an alternative to opioids for chronic pain may
confer similar, but modest, benefits to patients, and reduce the risk of opioid
overdose without substantially increasing costs."
https://www.liebertpub.com/doi/10.1089/can.2024.0120?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed
[5182]
On this side of the Atlantic, a
report by Sapphire Clinics on opioid prescription in the UK found that one in
seven (14%) chronic pain patients prescribed opioid medications claim they
became dependent or addicted, while strong side effects reportedly stopped one
in four (23%) from living a normal life.
57 million prescriptions for opioids
such as tramadol, codeine and fentanyl, were issued to UK patients in 2022, an
average of one 108 every minute.
https://www.sapphireclinics.com/wp-content/uploads/2023/06/opioid-campaign-whitepaper.pdf
[2852]
Marrinan et al (2024) in the UK
determined that increasing access to medical cannabis on the NHS for chronic
pain could save the state healthcare provider almost £4 billion annually, £729
per patient.
"An early cost-effectiveness model
was developed to estimate the impact of prescribing CBMPs alone and/or in
addition to analgesics, physiotherapy, and cognitive behavioral therapy for
chronic pain in the UK for 1 year.
"Results
Due to their comparative
effectiveness, CBMPs were found to be cost saving."
https://www.tandfonline.com/doi/full/10.1080/14737167.2024.2412248 [3629]
In "Perceived Efficacy, Reduced
Prescription Drug Use, and Minimal Side Effects of Cannabis in Patients with
Chronic Orthopedic Pain" (2022) Greis et al explain:
"Extant inventories for measuring
cannabis use were not designed to capture the medically relevant features of
cannabis use, but rather were designed to detect problematic use or cannabis use
disorder. Thus, we sought to capture the medically relevant features of cannabis
use in a population of patients with orthopedic pain and pair these data with
objective measures of pain and prescription drug use."
The results show:
"Medical cannabis use was associated
with clinical improvements in pain, function, and quality of life with
reductions in prescription drug use; 73% either ceased or decreased opioid
consumption and 31% discontinued benzodiazepines. … This work provides a direct
relationship between the initiation of cannabis therapy and objectively fewer
opioid and benzodiazepine prescriptions.”
https://www.liebertpub.com/doi/10.1089/can.2021.0088 [1828]
In Israel, Aviram et al (2021) found
“Patients with chronic pain, licensed
to use MC in Israel, reported weekly average pain intensity (primary outcome)
and related symptoms before and at 1, 3, 6, 9 and 12 months following MC
[medical cannabis] treatment initiation.. … 43% of the patients who had been
using analgesic medications prior to MC treatment initiation were no longer
using them. This was true for all classes of analgesic drugs including over the
counter analgesics, non-steroidal anti-inflammatory drugs, anticonvulsants and
antidepressants. As for opioid use, 24% and 20% of the participants who had been
using weak or strong opioids, respectively, at baseline stopped using them by
the time they reached the 12-month follow-up.”
https://pubmed.ncbi.nlm.nih.gov/33065768/ [1829]
In "Utilization of medicinal cannabis
for pain by individuals with spinal cord injury" Stillman et al found non-users
live in a different reality:
"Never users were less likely than
current and past users to agree that cannabis should be legalized (CU + PU =
98.00%; NU = 88.10%; χ2 = 10.92, p = .001) (Table 2) and more likely to believe
that cannabis is a 'gateway drug' (CU + PU = 7.40%; NU = 22.50%; χ2 = 12.80, p =
0.00), a 'very dangerous' drug (CU + PU = 1.30%; NU = 7.00%; χ2 = 5.90, p =
0.026), and that it is safer to take prescription pain killers than to use MC
(CU + PU = 4.00%; NU = 11.80%; χ2 = 5.91, p = 0.021). There was widespread
agreement among participants that cannabis could have medicinal effects (CU + PU
= 96.00%; NU = 95.30%; χ2 = 0.07, p = 1.00) and that its use carries either no
or only slight health risks (CU + PU = 91.20%; NU = 83.60%; χ2 = 3.61, p =
0.067). There were no significant differences in perceptions of social or legal
risks between the user groups."
But these authors did not find any
difference in pain interference. On the other hand:
"Subjects were asked to select from a
list of 33 possible effects that could be ascribed to MC and/or prescription
medications and that could be considered either positive, negative, or neutral.
On average, MC was assigned 7.6 positive effects while prescription medications
were assigned 5.35 (t = 3.9, df = 234; p = .000). Medicinal cannabis was
assigned an average of 6.0 negative effects while prescription medications were
assigned 9.9 (t = −3.76, df = 203; p = .001).
"When asked to compare the relative
efficacy of MC with that of other medications in providing symptom relief (98 CU
and 30 PU), 63.3% reported that cannabis works better than prescription
medications, 17.20% reported the opposite, and 10.20% answered that only
cannabis offered them relief (χ2 = 7.93, p = 0.047). When asked if they suffer
or had suffered from symptoms or conditions that had not been helped by MC,
35.20% replied “yes” (CU = 31.60%; PU = 46.70%; NS) and 64.80% replied “no” (CU
= 68.40%; PU = 53.30%; NS)."
“Among our subjects, over 90 percent
of CU [cannabis users] and PU [past users] reported “a little” or “great” relief
from symptoms with MC [medical cannabis] and 61.20 percent claimed that MC had
allowed them to reduce or discontinue use of other medications.”
https://www.nature.com/articles/s41394-019-0208-6.pdf [1830]
In "The Impact of Isolated Baseline
Cannabis Use on Outcomes Following Thoracolumbar Spinal Fusion: A Propensity
Score-Matched Analysis" Shah et al write:
"704 patients were identified (n=352
each), with comparable age, sex, race, primary insurance, Charlson/Deyo scores,
surgical approach, and levels fused between cohorts (all, p>0.05). Cannabis
users (versus non-users) incurred lower 90-day overall and medical complication
rates (2.4% vs. 4.8%, p=0.013; 2.0% vs. 4.1%, p=0.018). Cohorts had otherwise
comparable complication, revision, and readmission rates (p>0.05). Baseline
cannabis use was associated with a lower risk of 90-day medical complications
(OR=0.47, p=0.005). Isolated baseline cannabis use was not associated with
90-day surgical complications and readmissions, or two-year revisions.
"Isolated baseline cannabis use, in
the absence of any other diagnosed substance abuse disorders, was not associated
with increased odds of 90-day surgical complications or readmissions or two-year
revisions, though its use was associated with reduced odds of 90-day medical
complications when compared to non-users undergoing TLF (thoracolumbar spinal
fusion) for ASD (adult spinal deformity)."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9210439/ [1942]
In 2020's "The impact of cannabis
access laws on opioid prescribing", (2020) McMichael et al point out that
"...the number of opioid
prescriptions quadrupled in the first fifteen years of the new millennium."
and
"The five specialties that have the
highest prescribing rates, as measured by MMEs, reduce their opioid use by 28.3
percent when an RCL is passed and 6.9 percent when an MCL is passed."
"Table A1 reports the means of each
of our outcome variables across different cannabis legal regimes for all
specialties for which we have at least 2,000 provider-year observations."
"In general, we find consistent
evidence that both RCLs and MCLs reduce the use of prescription opioids. These
laws reduce the amount of annual MMEs prescribed by individual providers by 6.9
and 6.1 percent, respectively. However, our results are not unique to the MME
measure of opioid prescriptions, and both types of cannabis access laws
similarly reduce the total days supply of opioids, the number of patients to
whom providers prescribe opioids, and the probability that a provider prescribes
any opioids. Interestingly, while we find evidence that RCLs and MCLs reduce
opioid use across a wide array of medical (and other) specialties, the magnitude
of this reduction is not uniform across specialties."
Summary Statistics by Specialty Panel
A compares MMEs [morphine milligram equivalents] for All Providers and Providers
Not Subject to Any Cannabis Access Law. Only two of the 48 specialties listed -
Clinical Nurse Specialist and Physician Assistant - show modestly lower MMEs
where there is no cannabis access law, and so 46 were higher.
https://scholarship.law.ua.edu/cgi/viewcontent.cgi?article=1150&context=fac_working_papers
[1831]
"Our sample included 888 individuals
receiving treatment for chronic pain, of whom 99.4% received treatment with
prescription opioids or MC.
"Methods. Problematic use of
prescription opioids and MC was assessed using DSM-IV criteria, Portenoy’s
Criteria (PC), and the Current Opioid Misuse Measure (COMM) questionnaire.
Additional sociodemographic and clinical correlates of problematic use were also
assessed.
"Results. Among individuals treated
with prescription opioids, prevalence of problematic use of opioids according to
DSM-IV, PC, and COMM was 52.6%, 17.1%, and 28.7%, respectively. Among those
treated with MC, prevalence of problematic use of cannabis according to DSM-IV
and PC was 21.2% and 10.6%, respectively. Problematic use of opioids and
cannabis was more common in individuals using medications for longer periods of
time, reporting higher levels of depression and anxiety, and using alcohol or
drugs. Problematic use of opioids was associated with higher self-reported
levels of pain, and problematic use of cannabis was more common among
individuals using larger amounts of MC.
"Conclusions. Problematic use of
opioids is common among chronic pain patients treated with prescription opioids
and is more prevalent than problematic use of cannabis among those receiving MC.
Pain patients should be screened for risk factors for problematic use before
initiating long-term treatment for pain-control."
https://academic.oup.com/painmedicine/article-pdf/18/2/294/10452408/pnw134.pdf
[1832]
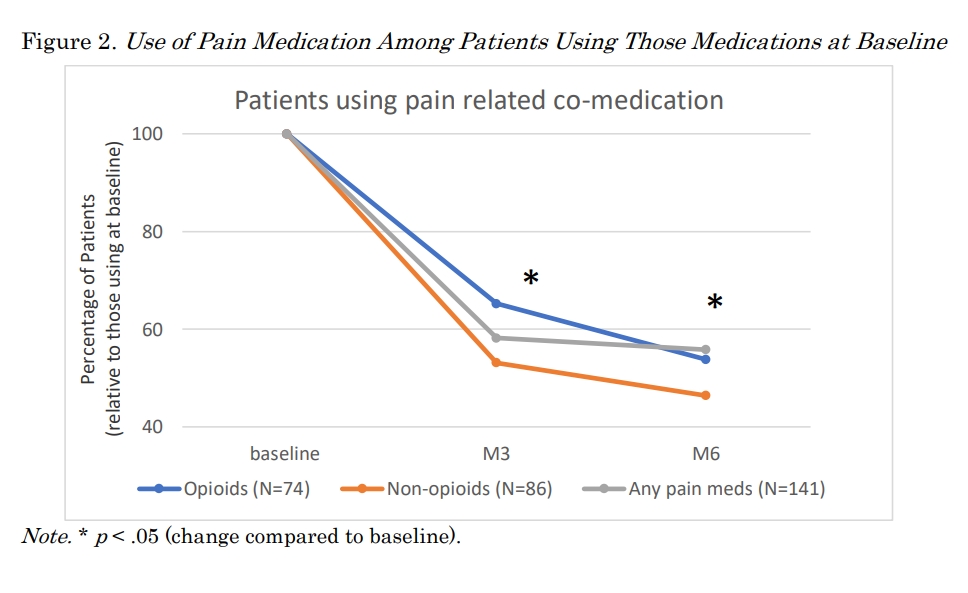
Another medical cannabis study by
Lucas et al (2021) focuses
"...on the impacts of cannabis on
prescription opioid use and quality of life over a 6-month period."
using 1145 patients and
"...a comprehensive cannabis use
inventory, the World Health Organization Quality of Life Short Form
(WHOQOL-BREF), and a detailed prescription drug questionnaire."
and
"Participants were 57.6% female, with
a median age of 52 years. Baseline opioid use was reported by 28% of
participants, dropping to 11% at 6 months. Daily opioid use went from 152 mg
morphine milligram equivalent (MME) at baseline to 32.2 mg MME at 6 months, a
78% reduction in mean opioid dosage. Similar reductions were also seen in the
other four primary prescription drug classes identified by participants, and
statistically significant improvements were reported in all four domains of the
WHOQOL-BREF."
and
"The high rate of cannabis use for
chronic pain and the subsequent reductions in opioid use suggest that cannabis
may play a harm reduction role in the opioid overdose crisis, potentially
improving the quality of life of patients and overall public health."
Other pharmaceuticals suffered
terribly as well:
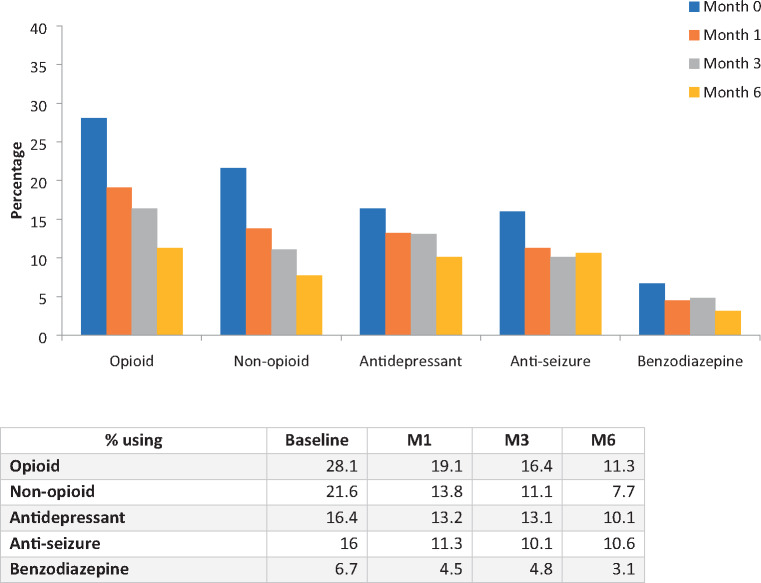
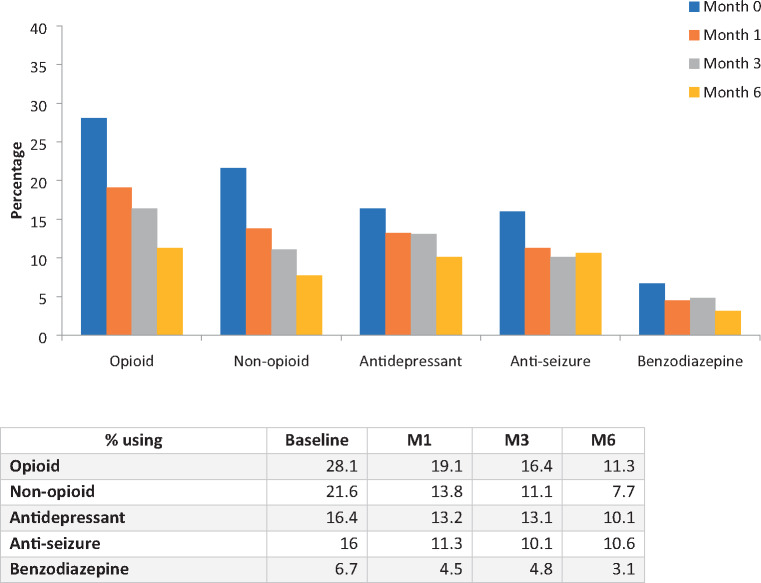
"Over 6 months, the percentage of
patients using non-opioid pain medications went from 21.6% (n=241) to 7.7%
(n=32), use of antidepressants declined from 16.4% (n=183) to 10.1% (n=42), use
of antiseizure medications went from 16% (n=178) to 10.6% (n=44), and
benzodiazepine use decreased from 6.7% of participants at baseline (n=75) to
3.1% at M6."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7971472/ [2815]
Dranitsaris et al (2021) examined
opioid prescribing before and after legalisation in Canada:
"Purpose: On 17 October 2018
recreational cannabis became legal in Canada, thereby increasing access and
reducing the stigma associated with its use for pain management. This study
assessed total opioid prescribing volumes and expenditures prior to and
following cannabis legalization.
"Methods: National monthly claims
data for public and private payers were obtained from January 2016 to June 2019.
The drugs evaluated consisted of morphine, codeine, fentanyl, hydrocodone,
hydromorphone, meperidine, oxycodone, tramadol, and the non-opioids gabapentin
and pregabalin. All opioid volumes were converted to a mean morphine equivalent
dose (MED)/claim, which is analogous to a prescription from a physician.
Gabapentin and pregabalin claims data were analyzed separately from the opioids.
Time-series regression modelling was undertaken with dependent variables being
mean MED/claim and total monthly spending. The slopes of the time-series curves
were then compared pre- versus post-cannabis legalization.
"Results: Over the 42-month period,
the mean MED/claim declined within public plans (p < 0.001). However, the
decline in MED/claim was 5.4 times greater in the period following legalization
(22.3 mg/claim post vs. 4.1 mg/claim pre). Total monthly opioid spending was
also reduced to a greater extent post legalization ($Can267,000 vs. $Can95,000
per month). The findings were similar for private drug plans; however, the
absolute drop in opioid use was more pronounced (76.9 vs. 30.8 mg/claim). Over
the 42-month period, gabapentin and pregabalin usage also declined.
"Conclusions: Our findings support
the hypothesis that easier access to cannabis for pain may reduce opioid use for
both public and private drug plans."
https://pubmed.ncbi.nlm.nih.gov/33491149/ [2143]
According to Beasley and Dundas
(2024) in "Recreational cannabis dispensary access effects on prescription
opioid use and mortality", in Oregon:
"Results suggest that communities
located closer to recreational dispensaries are associated with lower rates of
prescription opioids per capita. We also show that reasonable bounds to our
primary specification suggest communities located within a mile from a
recreational dispensary have prescription opioid rates per capita that are
1.0–3.9 percent lower than surrounding communities."
The study acknowledges that while
opioid-related mortality rates appeared unaffected by proximity to retail
marijuana, it’s possible that other measures of opioid harms, for example
hospitalizations, may nevertheless show an impact.
“While mortality rates do not appear
to be driven by changes in cannabis access,” it says, “hospitalizations related
to overdoses may be impacted. An extension of this work assessing
hospitalizations in lieu of mortality…may yield further insight.”
Authors said in the email to
Marijuana Moment that the issue of hospitalizations “was raised during peer
review of the article and our discussion in the paper on hospitalizations is
meant to convey that mortality reduction is just one metric that could be
impacted by reduced opioid prescriptions.”
“For example, it may be possible that
the same number of people succumb to opioid misuse, while fewer people are
hospitalized,” they added.
https://www.sciencedirect.com/science/article/abs/pii/S016604622400067X?via%3Dihub
[3128]
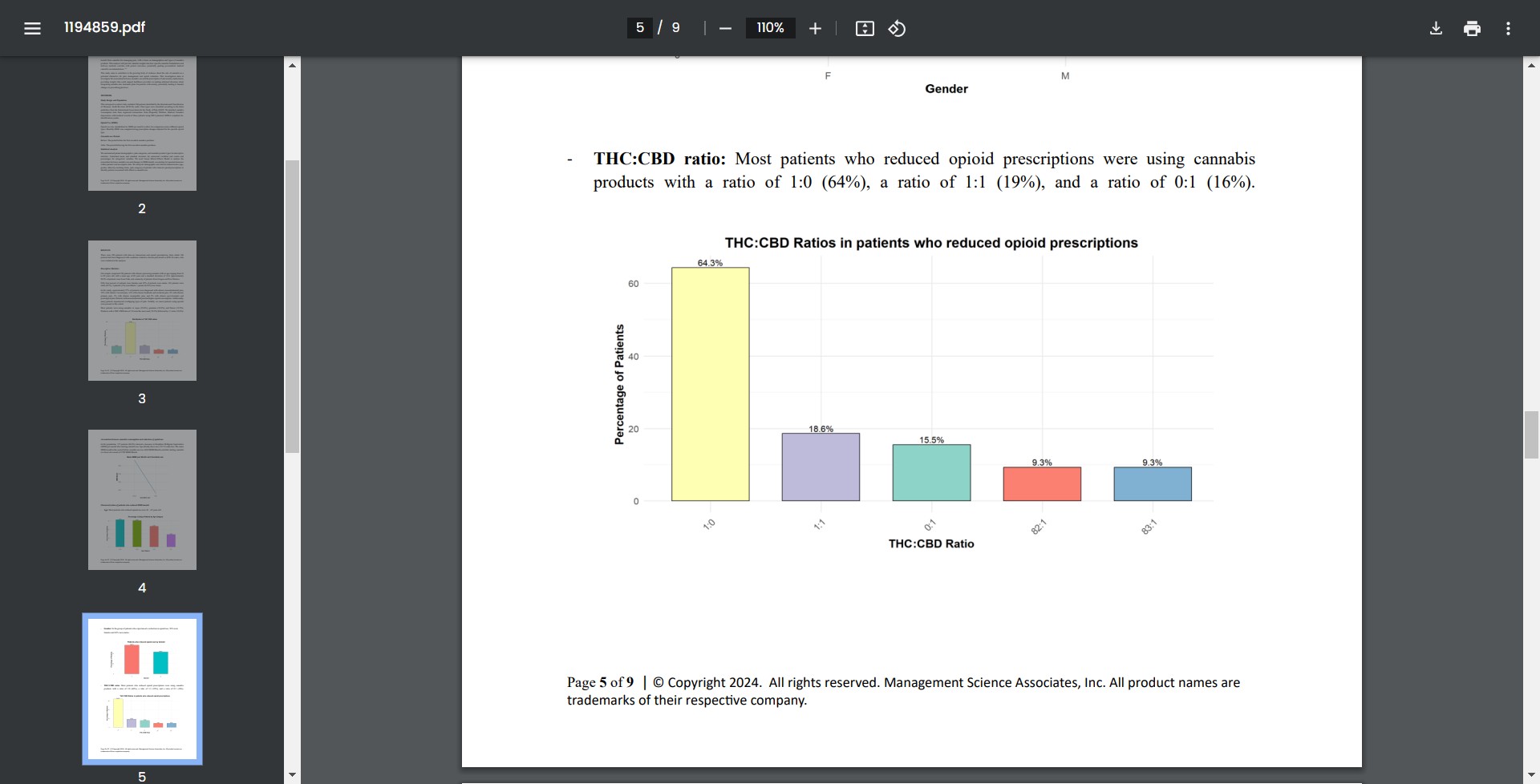
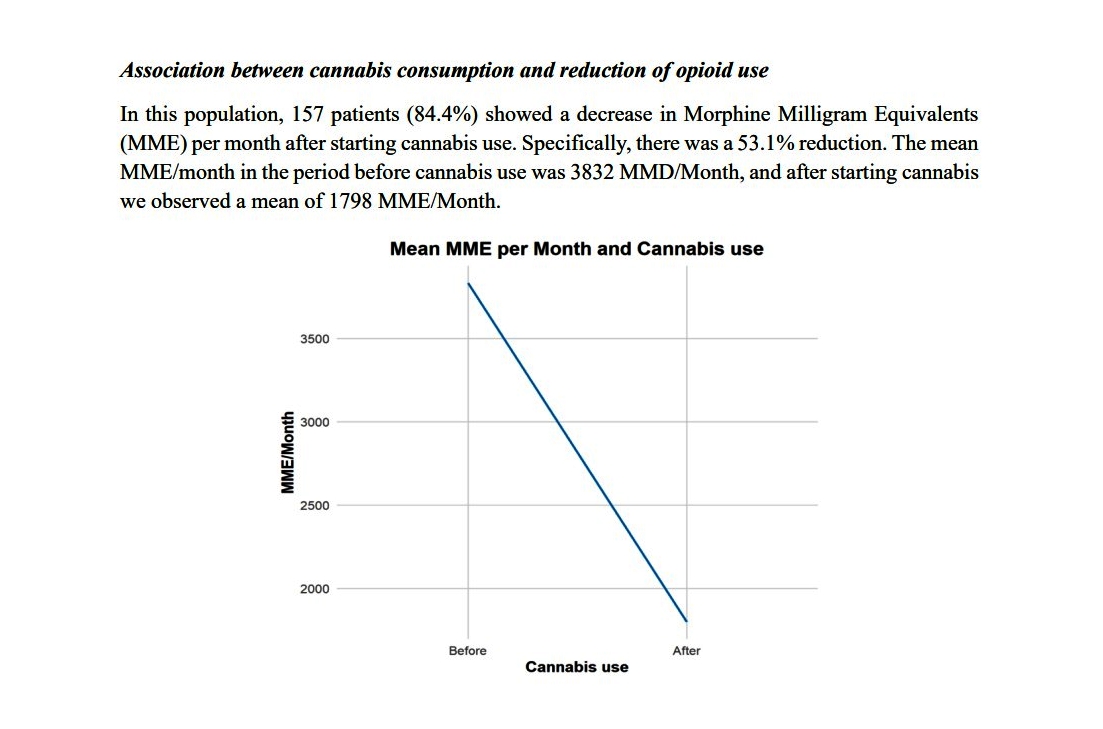
In Utah, most patients who reduced
opioid prescriptions were using cannabis products with a ratio of 1:0 (64%), a
ratio of 1:1 (19%) and 0:1 (16%):
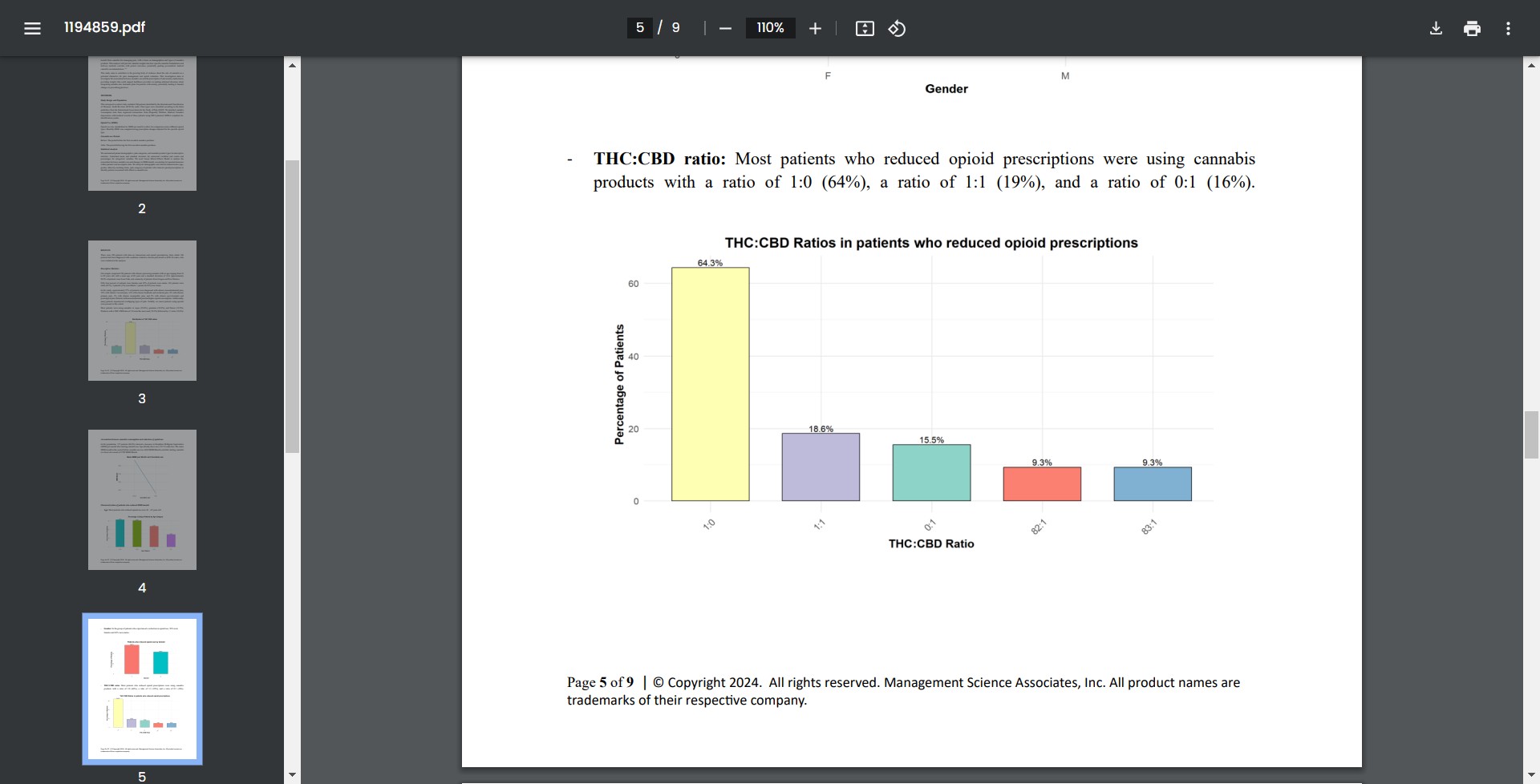
84% showed a decrease in Morphine
Milligram Equivalents (MME) per month after starting cannabis use.
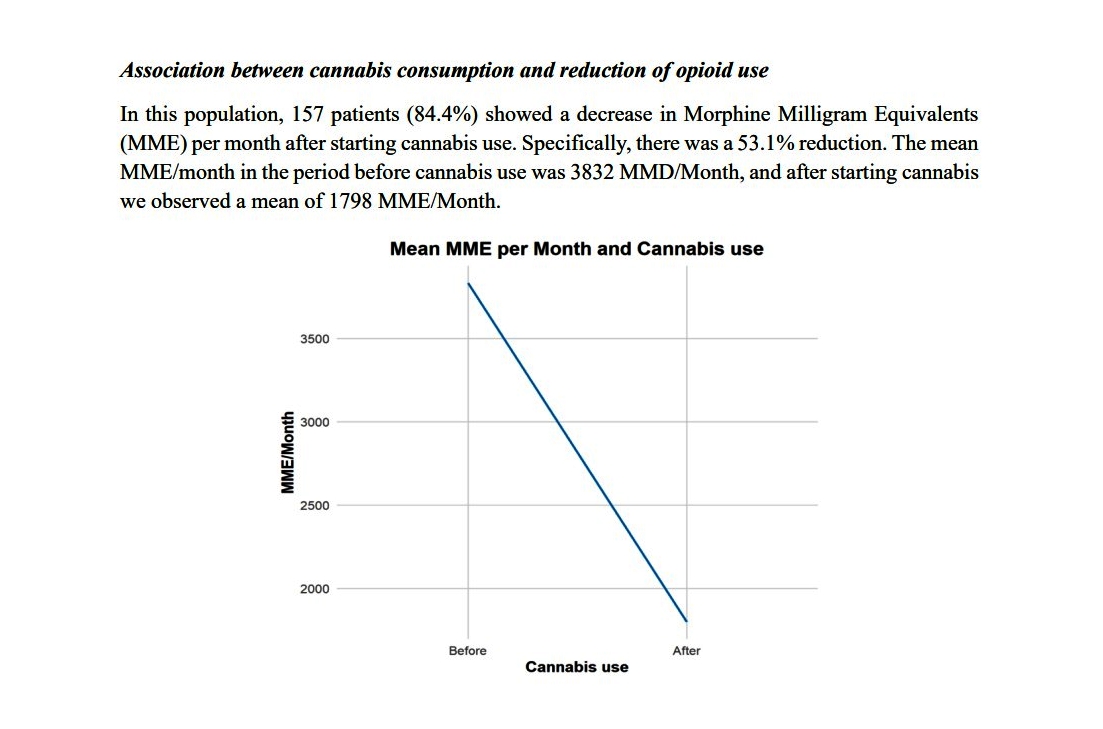
https://www.utah.gov/pmn/files/1194859.pdf [3742]
In Israel, Feingold et al examined
"Depression and anxiety among chronic pain patients receiving prescription
opioids and medical marijuana"...or both:
"Prevalence of depression among
patients in the OP (opioids), MM (medical marijuana) and OPMM groups was 57.1%,
22.3% and 51.4%, respectively and rates of anxiety were 48.4%, 21.5% and 38.7%,
respectively. … Levels of depression and anxiety are higher among chronic pain
patients receiving prescription opioids compared to those receiving MM. Findings
should be taken into consideration when deciding on the most appropriate
treatment modality for chronic pain, particularly among those at risk for
depression and anxiety."
https://www.ncbi.nlm.nih.gov/pubmed/28453948 [1833]
Hsu and Kovács (2021) reported an
"Association between county level cannabis dispensary counts and opioid related
mortality rates in the United States: panel data study" of 812 counties in the
United States in the 23 states that allowed legal forms of cannabis dispensaries
to operate by the end of 2017.
"Participants The study used US mortality data from the Centers for Disease
Control and Prevention combined with US census data and data from Weedmaps.com
on storefront dispensary operations. Data were analyzed at the county level by
using panel regression methods.
"Main outcome measure The main outcome measures were the log transformed, age
adjusted mortality rates associated with all opioid types combined, and with
subcategories of prescription opioids, heroin, and synthetic opioids other than
methadone. The associations of medical dispensary and recreational dispensary
counts with age adjusted mortality rates were also analyzed.
"Results County level dispensary count (natural logarithm) is negatively related
to the log transformed, age adjusted mortality rate associated with all opioid
types (β=−0.17, 95% confidence interval −0.23 to −0.11). According to this
estimate, an increase from one to two storefront dispensaries in a county is
associated with an estimated 17% reduction in all opioid related mortality
rates. Dispensary count has a particularly strong negative association with
deaths caused by synthetic opioids other than methadone (β=−0.21, 95% confidence
interval −0.27 to −0.14), with an estimated 21% reduction in mortality rates
associated with an increase from one to two dispensaries. Similar associations
were found for medical versus recreational storefront dispensary counts on
synthetic (non-methadone) opioid related mortality rates.
"Conclusions Higher medical and recreational storefront dispensary counts are
associated with reduced opioid related death rates, particularly deaths
associated with synthetic opioids such as fentanyl. While the associations
documented cannot be assumed to be causal, they suggest a potential association
between increased prevalence of medical and recreational cannabis dispensaries
and reduced opioid related mortality rates. This study highlights the importance
of considering the complex supply side of related drug markets and how this
shapes opioid use and misuse.
https://www.bmj.com/content/372/bmj.m4957 [4778]
Looking at cannabis use for pain management
and harm reduction, Kitchen et al (2025) report:
"Between June 2014 and May 2022, 2340 PWUD were initially recruited and of those
1242 PWUD reported chronic pain, use of unregulated opioids and completed at
least two follow-up visits. Of these 1242 participants, 764 experienced a
cessation event over 1038.2 person-years resulting in a cessation rate of 28.5
per 100 person-years (95% confidence interval [CI] 25.4-31.9). Daily cannabis
use was positively associated with opioid cessation (adjusted hazard ratio 1.40,
95% CI 1.08-1.81; p = 0.011). In the sex-stratified sub-analyses, daily cannabis
use was significantly associated with increased rates of opioid cessation among
males (adjusted hazard ratio 1.50, 95% CI 1.09-2.08; p = 0.014)."
https://pubmed.ncbi.nlm.nih.gov/40011075/ [5174]
Steuart et al (2025) took a long-term look at "Recreational Cannabis Laws and
Fills of Pain Prescriptions in the Privately Insured":
"Using data from a national sample of commercially insured adults, we examine
the effect of recreational cannabis legalization (through two sequential
policies) on prescribing of opioids, NSAIDS, and other pain medications by
implementing synthetic control estimations and constructing case-study level
counterfactuals for the years 2007-2020.
"Results:
Overall, we find recreational cannabis legalization is associated with a
decrease in opioid fills among commercially insured adults in the U.S., and we
find evidence of a compositional change in prescriptions of pain medications
more broadly. Specifically, we find marginally significant increases in
prescribing of non-opioid pain medications after recreational cannabis becomes
legal in some states. Once recreational cannabis dispensaries open, we find
statistically significant decreases in the rate of opioid prescriptions (13%
reduction from baseline, p < .05) and marginally significant decreases in the
average daily supply of opioids (6.3% decrease, p < .10) and number of opioid
prescriptions per patient (3.5% decrease, p < .10).
"Conclusions:
These results suggest that substitution of cannabis for traditional pain
medications increases as the availability of recreational cannabis increases.
There appears to be a small shift once recreational cannabis becomes legal, but
we see stronger results once users can purchase cannabis at recreational
dispensaries. The decrease in opioids and marginal increase in non-opioid pain
medication may reflect patients substituting opioids with cannabis and
non-opioid pain medications, either separately or concomitantly. Reductions in
opioid prescription fills stemming from recreational cannabis legalization may
prevent exposure to opioids in patients with pain and lead to decreases in the
number of new opioid users, rates of opioid use disorder, and related harms."
https://pmc.ncbi.nlm.nih.gov/articles/PMC11831899/ [4911]
Drake et al of the University of
Pittsburgh’s School of Public Health found "a significant reduction in
pharmacy-based codeine distribution in states that have legalized recreational
cannabis use. The finding is promising from a public health policy perspective
because misuse of prescription opioids annually contributes to more than 10,000
overdose deaths."
and
"The study is believed to be among
the first to separately examine the impact of recreational cannabis laws on
shipments of opioids to hospitals, pharmacies and other endpoint distributors.
Previous studies have focused on medical cannabis laws or use of opioids by
subsets of consumers, such as Medicaid beneficiaries."
and
"Key findings from states that passed
recreational cannabis laws:
"A 26% reduction in pharmacy-based
distribution of codeine and as much as a 37% reduction after recreational
cannabis laws have been in effect for four years.
"Minimal impact on distribution of
other opioids such as oxycodone, hydrocodone and morphine in any setting.
"Minimal impact on codeine
distribution by hospitals, which often have less permissive policies than
pharmacies."
"'This finding is particularly
meaningful,' said senior author Coleman Drake of the University of Pittsburgh’s
School of Public Health. 'Where previous studies have focused on more potent
opioids, codeine is a weaker drug with a higher potential for addiction. It
indicates people may be obtaining codeine from pharmacies for misuse, and that
recreational cannabis laws reduce this illicit demand.'"
https://news.cornell.edu/stories/2023/01/when-recreational-cannabis-legal-codeine-demand-drops
[2037]
B. Karmakar is an Assistant Professor
in the Department of Statistics, University of Florida, G. Mukherjee is an
Associate Professor in the Department of Data Sciences & Operations, University
of Southern California and W. Kar is an Assistant Professor of Purdue
University. Karmakar, Mukherjee and Kar (2023) studied the "Effect of Marijuana
Legalization on Direct Payments to Physicians by Opioid Manufacturers" and say:
"Our analysis finds a significant
decrease in direct payments from opioid manufacturers to pain medicine
physicians as an effect of MML passage. We provide evidence that this decrease
is due to the availability of medical marijuana as a substitute. Additionally,
physicians in states with an MML are prescribing fewer opioids. Finally, the
substitution effect is comparatively higher for female physicians and in
localities with higher white, less affluent, and more working-age populations."
As they explain:
"In the wake of this evolving pain
management paradigm, physicians must remain updated on drugs for appropriate
patient care. Without the latest information regarding the drugs, physicians may
be unable to prescribe opioids appropriately for pain management (Guo et al.,
2021). There is significant concern that a subsequent decrease in opioid
prescription could lead to opioid being a niche product or, in the extreme,
could potentially lead to severely diminished usage of opioids (Feinberg, 2019,
Szalavitz, 2023). Further, as a cascading effect, it can negatively affect
research and development on opioids as well as decrease in the number of opioid
manufacturers. Therefore, opioid manufacturers use different forms of
interactions to engage with physicians on a regular basis. One of the most
common conduits to facilitate such interactions is through direct payments to
physicians from opioid manufacturers (Jones and Ornstein, 2016, Schwartz and
Woloshin, 2019). These direct payments may be in the form of consulting and
speaker fees, conference travel reimbursements, or meal vouchers."
and
"...due to the 'Sunshine Act,'
pharmaceutical manufacturers are now mandated by law to report such payments
(Richardson et al., 2014). The act was a federal response to concerns of
potential conflict of interest in physicians accepting these payments, the
subsequent possibility of bias in treatment, and rising health-care costs (Carey
et al., 2021, DeJong et al., 2016, Engelberg et al., 2014, Jones and Ornstein,
2016). In September 2014, the first batch of data was made public. This dataset
contains the dollar value of the gift/payment that transpired between a named
physician and a named pharmaceutical manufacturer, associated products for their
interaction, and payment date."
Using a customised synthetic control
method:
"Our primary analysis considers all
pain medicine physicians from 13 states, of which three (PA, OH, LA) were
‘treated’ states that passed an MML in the second quarter of 2016. The method,
described in Section 3.4, produces synthetic
controls for each physician in the treated states using physicians in the
control states, and likewise produces synthetic counterparts for each physician
in the control states using physicians in the treated states."
So
"The results reported in Table 4 show
a significant negative correlation between an increase in marijuana patients in
preceding period as well as presence of a marijuana dispensary with
opioid-prescribing physician payment; however, there is no significant
association between physician payment and change in marijuana patients in the
following period. These results provide us with further support that the
substitution effect of marijuana is indeed the dominating factor in reducing
payments to pain medicine physicians post-passage of MML."
Some tears are necessary for the
"opioids ecosystem":
"Our study finds a significant
decrease in financial interactions between opioid manufacturers and physicians
as an effect of MML passage. The finding that the opioid manufacturers in states
that passed MML are stepping away from this particular form of interaction is
concerning, for such activity can significantly affect the opioids ecosystem."
But back with the patients
themselves:
"Analyzing the annual prescription
data (mentioned in Section 2), we found that, in 2015, they prescribed 49% more
opioids than non-opioids in 30 days’ fill and a similar 49% more days of
prescription for opioid vs non-opioid. From 2015 to 2017, in the states not
passing an MML, 30 days’ fill of opioid vs non-opioid remained flat at a 1.38:1
ratio. However, in the states passing an MML, from 2015 to 2017, 30 days’ fill
of opioid vs non-opioid decreased from a 1.57:1 ratio to a 1.52:1 ratio. The
ratios for the number of days of prescription in the MML states also decreased
from a 1.57:1 ratio in 2015 to a 1.52:1 ratio in 2017. In particular, the
pattern of opioid vs non-opioid prescriptions did not change in the control
states, while there was a relative decrease in opioid prescriptions in the MML
states from 2015 to 2017."
https://people.clas.ufl.edu/bkarmakar/files/2023/03/physicians_opioids.pdf
[2328]
In "'I got a bunch of weed to help me
through the withdrawals': Naturalistic cannabis use reported in online opioid
and opioid recovery community discussion forums" Meachem et al (2022)
"...extracted all posts mentioning
cannabis-related keywords (e.g., 'weed', 'cannabis', “marijuana”) from December
2015 through August 2019 from an opioid use subreddit and an opioid recovery
subreddit. … The most frequent phrases from the recovery subreddit referred to
time without using opioids and the possibility of using cannabis as a
‘treatment.’ … The most common motivations for using cannabis were to manage
opioid withdrawal symptoms in the recovery subreddit, often in conjunction with
anti-anxiety and GI-distress 'comfort meds.' … Despite limitations in
generalizability from pseudonymous online posts, this examination of reports of
naturalistic cannabis use in relation to opioid use identified withdrawal
symptom management as a common motivation.”
https://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0263583&type=printable
[1834]
In 2021's "The association between
cannabis use and outcome in pharmacological treatment for opioid use disorder"
Rosic et al in the Harm Reduction Journal
"Participants receiving
pharmacological treatment for OUD (n = 2315) were recruited from community-based
addiction treatment clinics in Ontario, Canada, and provided information on
past-month cannabis use (self-report). Participants were followed for 3 months
with routine urine drug screens in order to assess opioid use during treatment.
We used logistic regression analysis to explore (1) the association between any
cannabis use and opioid use during treatment, and (2) amongst cannabis-users,
specific cannabis use characteristics associated with opioid use. … We found
that amongst cannabis users, those who use cannabis daily are less likely to
have opioid use than people who use cannabis occasionally. This association was
present for both men and women. … Future studies should further examine specific
characteristics and patterns of cannabis use that may be protective or
problematic in MAT [medication-assisted treatment]."
Sex differences were observed:
"Interaction analysis revealed no
significant moderating effect of sex on our cannabis use characteristics of
interest (age of onset of cannabis use by sex: OR = 0.99, 95% CI 0.94, 1.05,
p = 0.725; daily cannabis use by sex: OR = 0.92, 95% CI 0.53, 1.57, p 0.748;
side effects from cannabis by sex: OR = 1.53, 95% CI 0.93, 2.50, p = 0.092;
marijuana cravings score by sex: OR = 1.01, 95% CI 0.99, 1.03, p = 0.100). Using
subgroup analysis by sex, we found the association between reporting
cannabis-related side effects and lower odds of opioid use to hold for men
(OR = 0.55, 95% CI 0.40, 0.75, p < 0.001), but not for women (OR = 0.86, 95% CI
0.59, 1.26, p = 0.442). Additionally, for women, but not men, higher marijuana
cravings score was associated with increased odds of opioid use (scaled for each
10-point increase in score: OR = 1.14, 95% CI 1.01, 1.28, p = 0.034)."
Overall
"For cannabis users, daily cannabis
use was associated with lower odds of opioid use, when compared with occasional
use (OR = 0.61, 95% CI 0.47–0.79, p < 0.001) as was older age of onset of
cannabis use (OR = 0.97, 95% CI 0.94, 0.99, p = 0.032), and reporting
cannabis-related side effects (OR = 0.67, 95% CI 0.51, 0.85, p = 0.001)."
And adopting a rather melancholy
angle, they go on:
"Altogether, 75% of cannabis users
perceived no impact of cannabis on their OUD treatment."
https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-021-00468-6
[1835]
For Johns Hopkins University School
of Medicine, Bergeria et al (2020)
"Two hundred individuals recruited
through Amazon Mechanical Turk with past month opioid and cannabis use and
experience of opioid withdrawal completed the survey. Participants indicated
which opioid withdrawal symptoms improved or worsened with cannabis use and
indicated the severity of their opioid withdrawal on days with and without
cannabis. … 62.5% of 200 participants had used cannabis to treat withdrawal.
Participants most frequently indicated that cannabis improved: anxiety, tremors,
and trouble sleeping. … These results show that cannabis may improve opioid
withdrawal symptoms and that the size of the effect is clinically meaningful."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7212528/ [1836]
Wiese and Wilson-Poe reviewed the
evidence in 2018.
"The endocannabinoid and opioidergic
systems are known to interact in many different ways, from the distribution of
their receptors to cross-sensitization of their behavioral pharmacology.
Cannabinoid-1 (CB1) receptors and mu opioid receptors (MORs) are distributed in
many of the same areas in the brain, including but not limited to the
periaqueductal gray, locus coeruleus, ventral tegmental area (VTA), nucleus
accumbens, prefrontal cortex (PFC), central amygdala (CeA), bed nucleus of stria
terminalis (BNST), caudate putamen (CP), substantia nigra, dorsal hippocampus,
raphe nuclei, and medial basal hypothalamus. The extent of this overlapping
expression and frequent colocalization of the CB1 and MOR provide clear
morphological underpinnings for interactions between the opioid and cannabinoid
systems in reward and withdrawal."
Besides,
"Interestingly, microinjections of
CB1 agonists into the medial PFC creates an aversion to doses of morphine that
are normally rewarding (CPP), while CB1 antagonism in this brain region creates
a rewarding effect of subthreshold morphine doses."
"The evidence summarized in this
article demonstrates the potential cannabis has to ease opioid withdrawal
symptoms, reduce opioid consumption, ameliorate opioid cravings, prevent opioid
relapse, improve OUD treatment retention, and reduce overdose deaths. … The
compelling nature of these data and the relative safety profile of cannabis
warrant further exploration of cannabis as an adjunct or alternative treatment
for OUD."
https://www.liebertpub.com/doi/10.1089/can.2018.0022 [1837]
In a 2025 paper "Cannabidiol attenuates
heroin seeking in male rats associated with normalization of discrete
neurobiological signatures within the nucleus accumbens with subregional
specificity" from Chisholm et al of the Icahn School of Medicine at Mount Sinai,
Departments of Neuroscience, Psychiatry; Addiction Institute of Mount Sinai:
"Heroin-trained animals exhibited high levels of cue-induced heroin-seeking
behavior. Importantly, CBD attenuated cue-induced heroin-seeking behaviors.
Postmortem RNA-sequencing of the NAcC and NAcS revealed shared transcriptomic
alterations the NAc subregions in response to heroin, with a more robust impact
of heroin in the NAcS. Though CBD had minimal impact on the heroin-induced
perturbations in the NAcC, it normalized components of the transcriptomic
signature altered by heroin in both NAc subregions including transcripts that
correlated with heroin-seeking behavior. In contrast, CBD normalized a
particular subset of NAcS genes that correlated to heroin-seeking behavior.
Those genes were specifically linked to the extracellular matrix, astrocyte
function, and their upstream regulators related to immune function."
https://www.sciencedirect.com/science/article/abs/pii/S0006322325014623
[5449]
Raman et al examined codeine sales at
pharmacies in US states which had passed recreational cannabis laws as of
November 2022.
"We implement two-way fixed-effects
regressions and leverage variation from eleven U.S. states that adopted a
recreational cannabis law (RCL) between 2010 and 2019. We find that RCLs lead to
a reduction in codeine dispensed at retail pharmacies. Among prescription
opioids, codeine is particularly likely to be used non-medically. Thus, the
finding that RCLs appear to reduce codeine dispensing is potentially promising
from a public health perspective."
"We are the first study, to our
knowledge, to leverage ARCOS data which details distribution by
endpoint—pharmacies, hospitals, specialists, and narcotic treatment programs—to
study the effects of" recreational legalization, the authors wrote.
They further said that the effect of
legalization on codeine prescribing became more pronounced over years,
"increasing from -17.5 percent one year after RCL implementation to -37.3
percent four years after implementation."
https://onlinelibrary.wiley.com/doi/10.1002/hec.4652 [2057]
A commonplace reason for using
marijuana in Ptuj is as an exit drug. Even without any LSD or mushrooms, a
proportion of the alcoholically-inclined realise at some point that things are
not getting better. When you go drinking, it starts out good and goes downhill
from there. Perhaps if I have some more it will get even better. It doesn't. In
the long run most fortunately realise that the alcohol sweet spot really only
lasts a very short time, and the older you get the shorter that sweet spot is.
If you want to use marijuana as an
exit drug that's not a medical issue. You didn't need a prescription to get the
drug that caused the problem, but you can't get one for the cure, because it's
illegal. Clearly this interferes with the desire of the self-aware person in
trouble with alcohol who wants an easy path to harm reduction."
A 2021 paper from Scripps Research
Institute and the University of California report, which only looked at CBD,
reports:
"Cannabidiol reduces craving in
animal models of alcohol and cocaine use."
because...
"CBD prevented rats from exhibiting
somatic signs of withdrawal and hyperalgesia during acute and protracted
abstinence. There was no dose-response observed for CBD, suggesting a ceiling
effect at the doses used and the potential for lower effective doses of CBD."
https://pubmed.ncbi.nlm.nih.gov/33909102/ [839]
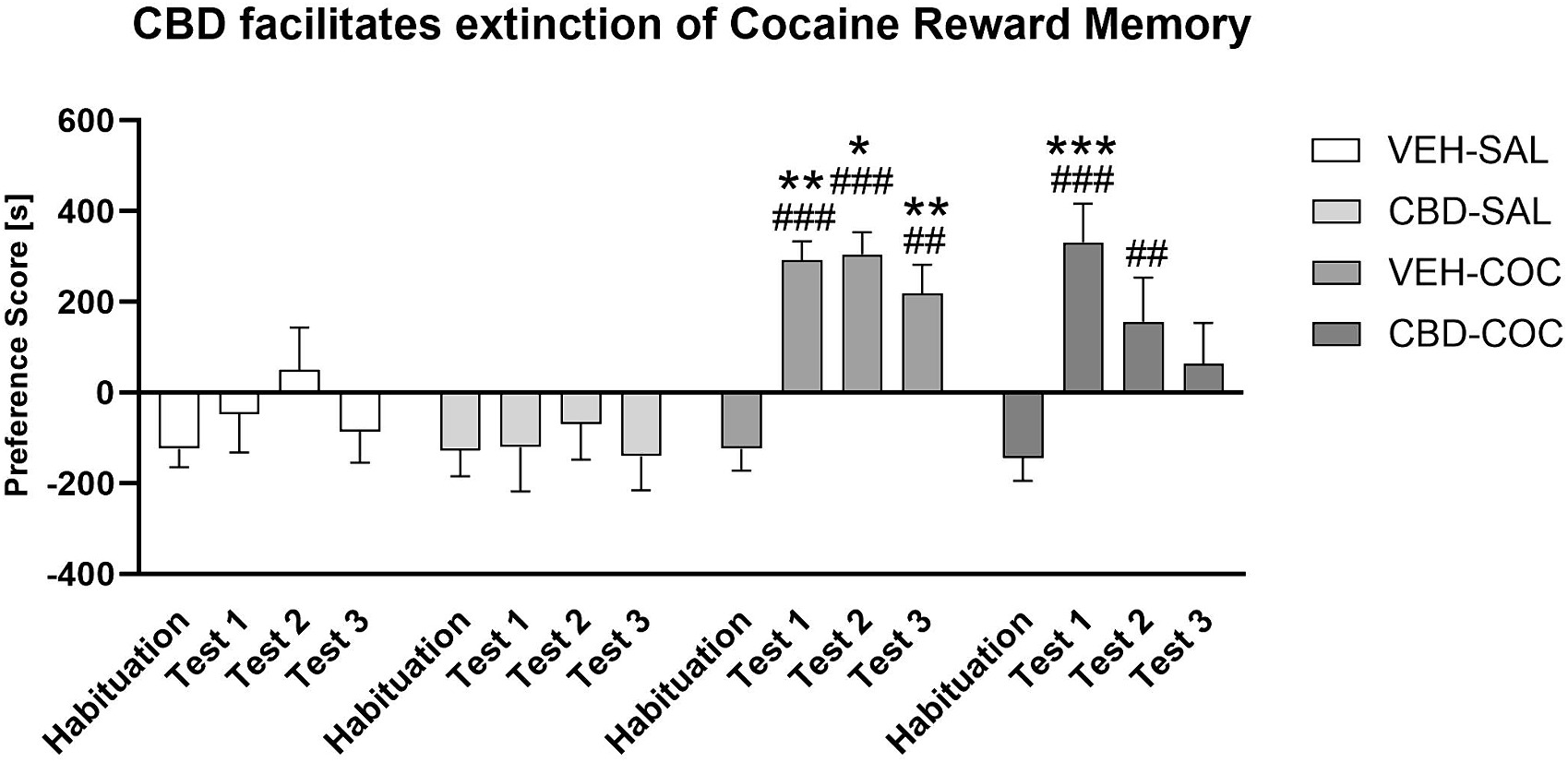
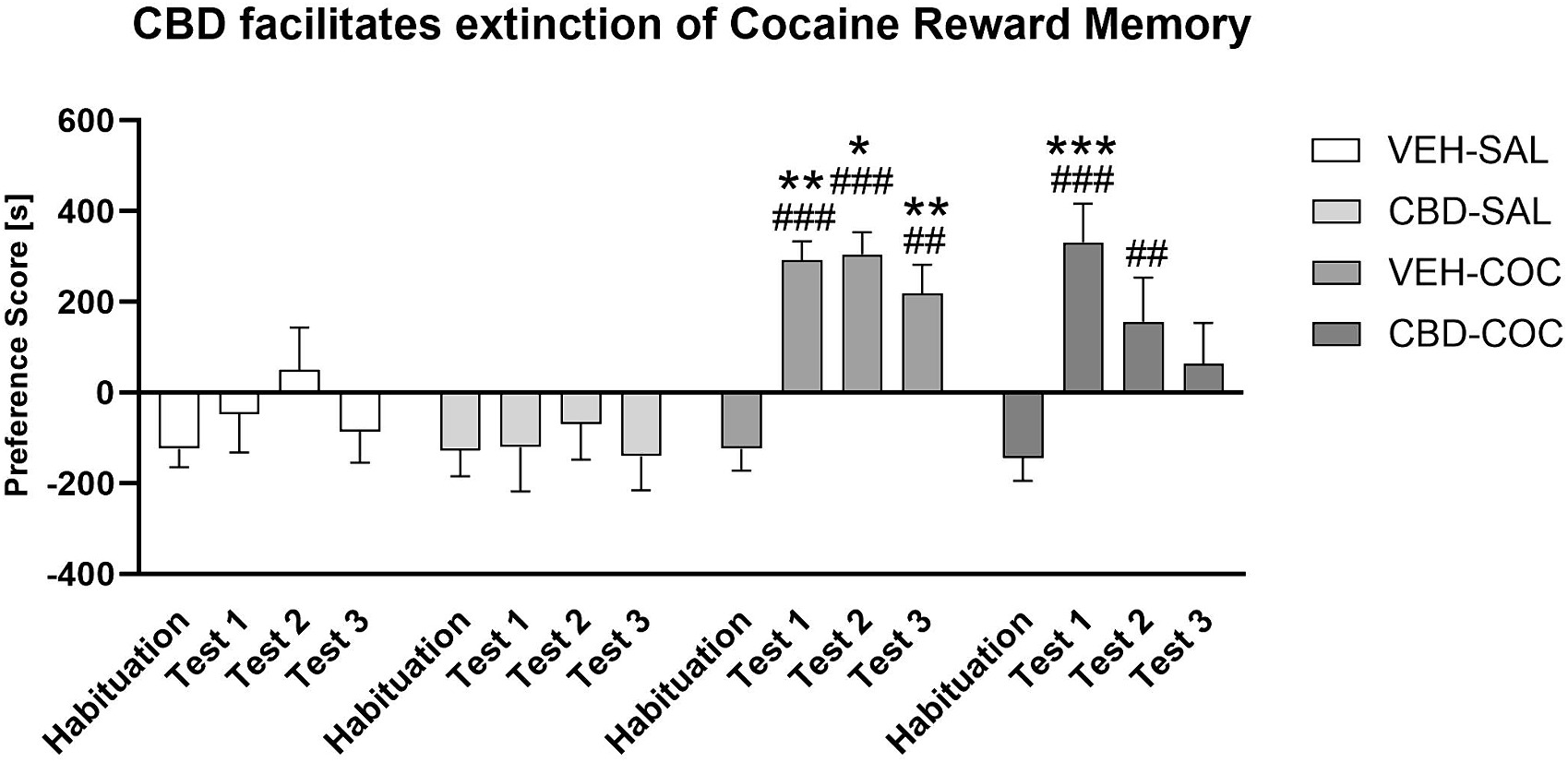
"Cannabidiol (CBD) facilitates
cocaine extinction and ameliorates cocaine-induced changes to the gut microbiome
in male C57BL/6JArc mice" say Chesworth et al (2024).
"Cocaine use disorder (CUD) is a
global health problem with no approved medications. One potential treatment
target is the gut microbiome, but it is unknown if cocaine induces long-lasting
effects on gut microbes. A novel therapeutic candidate for CUD, cannabidiol
(CBD), can improve gut function in rodent models. It is possible that protective
effects of CBD against cocaine use are mediated by improving gut health. We
examined this question in this experiment. Cocaine conditioned place preference
(CPP) was conducted in adult male C57BL/6JArc mice. Mice were treated with
vehicle or 20 mg/kg CBD prior to all cocaine CPP sessions (N = 11–13/group).
Mice were tested drug free 1, 14 and 28 days after cessation of cocaine and CBD
treatment. Fecal samples were collected prior to drug treatment and after each
test session. Gut microbiome analyses were conducted using 16 s rRNA sequencing
and correlated with behavioural parameters. We found a persistent preference for
a cocaine-environment in mice, and long-lasting changes to gut microbe alpha
diversity. Cocaine caused persistent changes to beta diversity which lasted for
4 weeks. CBD treatment reduced cocaine-environment preference during abstinence
from cocaine and returned gut beta diversity measures to control levels. CBD
treatment increased the relative abundance of Firmicutes phyla and Oscillospira
genus, but decreased Bacteroidetes phyla and Bacteroides acidifaciens species.
Preference score in cocaine-treated mice was positively correlated with
abundance of Actinobacteria, whereas in mice treated with CBD and cocaine, the
preference score was negatively correlated with Tenericutes abundance. Here we
show that CBD facilitates cocaine extinction memory and reverses persistent
cocaine-induced changes to gut microbe diversity. Furthermore, CBD increases the
abundance of gut microbes which have anti-inflammatory properties. This suggests
that CBD may act via the gut to reduce the memory of cocaine reward. Our data
suggest that improving gut health and using CBD could limit cocaine abuse."
https://www.sciencedirect.com/science/article/pii/S0278584624000824?via%3Dihub
[3360]
Prohibition, if observed, makes it
harder for people giving up smoking and cocaine.
The Defence anticipates the Court will be interested
in obsessive craving. As Bönsch et al reveal in Human Molecular Genetics in
2005,
"Various studies have linked alcohol
dependence phenotypes to chromosome 4. One candidate gene is NACP (non-amyloid
component of plaques), coding for alpha synuclein. Recently, it has been shown
that alpha synuclein mRNA is increased in alcohol-dependent patients within
withdrawal state. This increase is significantly associated with craving,
especially obsessive craving. On the basis of these observations, the present
study analysed two polymorphic repeats within the NACP gene. We found highly
significant longer alleles of NACP-REP1 in alcohol-dependent patients compared
with healthy controls (Kruskal–Wallis test, χ2=99.5; df=3, P<0.001). In
addition, these lengths significantly correlate with levels of expressed alpha
synuclein mRNA (χ2=8.83; df=2, P=0.012). The present results point to a novel
approach for a genetic determination of craving, a key factor in the genesis and
maintenance not only of alcoholism but also of addiction in general."
https://academic.oup.com/hmg/article/14/7/967/626665?login=false [2978]
According to Hallbeck et al (2024) "Accumulation of alpha-synuclein pathology in
the liver exhibits post-translational modifications associated with Parkinson’s
disease"
"In previous work, we showed that human hepatocytes can take up α-syn assemblies
via the gap junction protein connexin-32 (Cx32). Furthermore, we found an
age-dependent accumulation of human α-syn pathology within the liver in multiple
animal models of PD (L61, (Thy-1)-h[A30P])), and MSA (MBP29). Importantly, the
accumulation of α-syn within the liver was not due to hepatic mRNA expression,
indicating that α-syn deposits are derived directly from the brain or indirectly
from other peripheral tissues. Moreover, we corroborated that α-syn pathology in
neuropathologically confirmed PD cases can be found to a higher degree than in
controls with no α-syn pathology in the brain. In the current report, we
investigated the presence of α-syn post-translational modifications (PTMs) in
the liver from aged (Thy-1)-h[A30P] mice (A30P). We now report the presence of
hallmark PTMs associated with PD, including tyrosine nitration (nY39),
phosphorylation (pY39, pS87 and pS129, Y133) and C-terminal truncation events
(X-122). Ex vivo, we demonstrate that human hepatocytes (HuH-7) degrade
pre-formed fibrils (PFF) more efficiently than oligomeric assemblies. However,
by increasing autophagy using the pharmacological inhibitor rapamycin, we could
enhance oligomeric α-syn degradation in a concentration-dependent manner.
Moreover, ex vivo we also observe several PTMs that have been demonstrated in
vivo. Taken together, our results demonstrate the presence of key pathological
modifications associated with PD, also present in the liver of a mouse model of
PD. Our findings suggest that α-syn aggregates are transported from the brain to
the liver in a modified state or upon arrival, they undergo specific PTMs to
facilitate their clearance and detoxification, suggesting a new role for the
liver in the clearance of PD-associated pathology."
https://www.cell.com/iscience/fulltext/S2589-0042(24)02675-0 [3903]
What are the effects of cannabis on
synuclein?
In "The Neuroprotective Effects of
Cannabis-Derived Phytocannabinoids and Resveratrol in Parkinson’s Disease: A
Systematic Literature Review of Pre-Clinical Studies" (2021) by Prakash and
Carter:
"A total of 1034 publications were
analyzed, of which 18 met the eligibility criteria for this review.
Collectively, the majority of PD rodent studies demonstrated that treatment with
CDCs or RSV produced a significant improvement in motor function and mitigated
the loss of dopaminergic neurons. Biochemical analysis of rodent brain tissue
suggested that neuroprotection was mediated by anti-oxidative,
anti-inflammatory, and anti-apoptotic mechanisms. This review highlights the
neuroprotective potential of CDCs and RSV for in vivo models of PD and therefore
suggests their potential translation to human clinical trials to either
ameliorate PD progression and/or be implemented as a prophylactic means to
reduce the risk of development of PD."
and
"Seven studies investigated the
effects of RSV and CDCs on neuroinflammation in rodent brain tissue of the
striatum and SNpc, and included neurotoxin models, a genetic model, as well as
specific induction of neuroinflammation via LPS treatment. The results of these
studies are summarized in Table 6 and have been divided by their intervention
group (BCP [β-caryophyllene], THCV [tetrahydrocannabivarin], and RSV
[resveratrol]), and then ascending year of study. Five studies showed increased
markers of microglia and astrocytes activation via quantification of glial
fibrillary acidic protein (GFAP) and ionized calcium-binding adaptor molecule 1
(Iba-1) protein or mRNA levels, and these were significantly reduced via
administration of THCV, BCP, or RSV. Inflammatory protein markers and their
complementary mRNA levels were significantly increased in the PD model groups
and this was significantly countered with BCP or RSV treatment. The suppressor
of cytokine signaling protein 1 (SOCS-1) was detected in α-synuclein transgenic
mice and was significantly upregulated by RSV treatment."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8699487/ [2979]
In "Neuroprotective effects of
cannabidiol on dopaminergic neurodegeneration and α-synuclein accumulation in C.
elegans models of Parkinson's disease" (2022) Muhammad et al found that:
"CBD at 0.025 mM (24.66 %), 0.05 mM
(52.41 %) and 0.1 mM (71.36 %) diminished DA neuron degenerations induced by
6-hydroxydopamine (6-OHDA), reduced (0.025, 27.1 %), (0.05, 38.9 %), (0.1, 51.3
%) food-sensing behavioural disabilities in BZ555, reduced 40.6 %, 56.3 %, 70.2
% the aggregative toxicity of α-Syn and expanded the nematodes' lifespan up to
11.5 %, 23.1 %, 28.8 %, dose-dependently....these findings supported CBD as an
anti-parkinsonian drug and may exert its effects by raising lipid depositions to
enhance proteasome activity and reduce oxidative stress via the antioxidative
pathway."
https://pubmed.ncbi.nlm.nih.gov/36108815/ [2980]
In Sao Paulo, Erustes et al (2025) found
"Cannabidiol induces autophagy via CB1 receptor and reduces α-synuclein
cytosolic levels":
"To investigate the participation of each cannabinoid receptor in the induction
of autophagy, cells were treated with selective cannabinoid agonists that
interact specifically with receptors of the human endocannabinoid system. In
this way, autophagic flux was evaluated in cells treated with agonists and
antagonists of cannabinoid receptors: ACEA/AM251 (10 µM/10 µM, CB1R),
GW405833/AM630 (1 µM/3 µM, CB2R) and capsaicin/capsazepine (10 µM/10 µM, TRPV1).
Cells were treated with these compounds for 4 h both in the presence or absence
of NH4Cl (10 mM added during the last hour of treatment), which is used as an
inhibitor of lysosomal degradation. In the groups treated with the agonist and
antagonist, the antagonists were added during the first 30 min, followed by the
addition of the agonists.
"The evaluation of autophagic flux demonstrated that compared with control cells
and cells treated with ACEA [Arachidonoyl 2-chloroethylamide] in the absence of
an inhibitor, cells stimulated with ACEA in the presence of NH4Cl accumulated
LC3-II (Fig. 3a). Autophagic flux was inhibited when cells were treated with
ACEA in the presence of AM251 (a CB1R antagonist); in this way, the addition of
an antagonist blocked the effect of the agonist on the induction of autophagy."
https://www.sciencedirect.com/science/article/pii/S0006899324006693?via%3Dihub
[3831]
Wang et al (2022) also found that:
"Cannabidivarin alleviates α-synuclein aggregation via DAF-16 in Caenorhabditis
elegans"
https://faseb.onlinelibrary.wiley.com/doi/abs/10.1096/fj.202200278RR [2981]
"DAF-16 is the sole ortholog of the FOXO family of transcription factors in the
nematode Caenorhabditis elegans....The gene has played a large role in research
into longevity and the insulin signalling pathway as it is located in C.
elegans, a successful ageing model organism."
https://en.wikipedia.org/wiki/Daf-16 [2984]
These studies point to the conclusion that cannabinoids inhibit synuclein.
Therefore they reduce cravings as well as inhibiting neuroinflammatory pathways:
"Glycine receptors are expressed mainly in Purkinje cells. In hyperammonemic
rats, enhanced glycinergic neurotransmission leads to reduced membrane
expression of ADAM17, resulting in increased surface expression and activation
of TNFR1 and of the associated NF-kB pathway. This increases the expression in
Purkinje neurons of TNFa, IL-1b, HMGB1, and glutaminase. Increased glutaminase
activity leads to increased extracellular glutamate, which increases
extracellular GABA. Increased extracellular glutamate and HMGB1 potentiate
microglial activation. Blocking glycine receptors with strychnine or
extracellular cGMP completely prevents the above pathway in hyperammonemic
rats."
And rats in this condition were used to test this because:
"Rats with chronic hyperammonemia reproduce the cognitive impairment and motor
in-coordination shown by cirrhotic patients with minimal hepatic encephalopathy
and are a good model to identify the underlying mechanisms and to test
treatments to improve them. Chronic hyperammonemia induces neuroinflammation
which alters glutamatergic and GABAergic neurotransmission in cerebellum and
hippocampus leading to cognitive and motor impairment.
https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-020-01941-y
[3832]
Wang et al (2022) also found that:
"Cannabidivarin alleviates
α-synuclein aggregation via DAF-16 in Caenorhabditis elegans"
https://faseb.onlinelibrary.wiley.com/doi/abs/10.1096/fj.202200278R [2981]
"DAF-16 is the sole ortholog of the
FOXO family of transcription factors in the nematode Caenorhabditis
elegans....The gene has played a large role in research into longevity and the
insulin signalling pathway as it is located in C. elegans, a successful ageing
model organism."
https://en.wikipedia.org/wiki/Daf-16 [2984]
These studies point to the conclusion that
cannabinoids inhibit synuclein. Therefore they reduce cravings as well as
inhibiting neuroinflammatory pathways. As Arenas et al (2020) of the Príncipe
Felipe Research Center in Valencia explain:
"Glycine receptors are expressed mainly in Purkinje cells. In hyperammonemic
rats, enhanced glycinergic neurotransmission leads to reduced membrane
expression of ADAM17, resulting in increased surface expression and activation
of TNFR1 and of the associated NF-kB pathway. This increases the expression in
Purkinje neurons of TNFa, IL-1b, HMGB1, and glutaminase. Increased glutaminase
activity leads to increased extracellular glutamate, which increases
extracellular GABA. Increased extracellular glutamate and HMGB1 potentiate
microglial activation. Blocking glycine receptors with strychnine or
extracellular cGMP completely prevents the above pathway in hyperammonemic
rats."
And rats in this condition were used to test this because:
"Rats with chronic hyperammonemia reproduce the cognitive impairment and motor
in-coordination shown by cirrhotic patients with minimal hepatic encephalopathy
and are a good model to identify the underlying mechanisms and to test
treatments to improve them. Chronic hyperammonemia induces neuroinflammation
which alters glutamatergic and GABAergic neurotransmission in cerebellum and
hippocampus leading to cognitive and motor impairment.
https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-020-01941-y
[3832]
In the main, however, study of
alpha-synucleinopathies is focussed on PD. A summary of the findings around
alpha-synuclein can be found in Table 1 (PD), and other alpha-synucleinopathies
in "Peripheral Tissues as a Possible Marker for Neurological Diseases and Other
Medical Conditions" by Jiménez-Jiménez et al (2023).
https://www.researchgate.net/publication/373232996_Alpha-Synuclein_in_Peripheral_Tissues_as_a_Possible_Marker_for_Neurological_Diseases_and_Other_Medical_Conditions/link/64e191cd14f8d173380c05fe/download[2982]
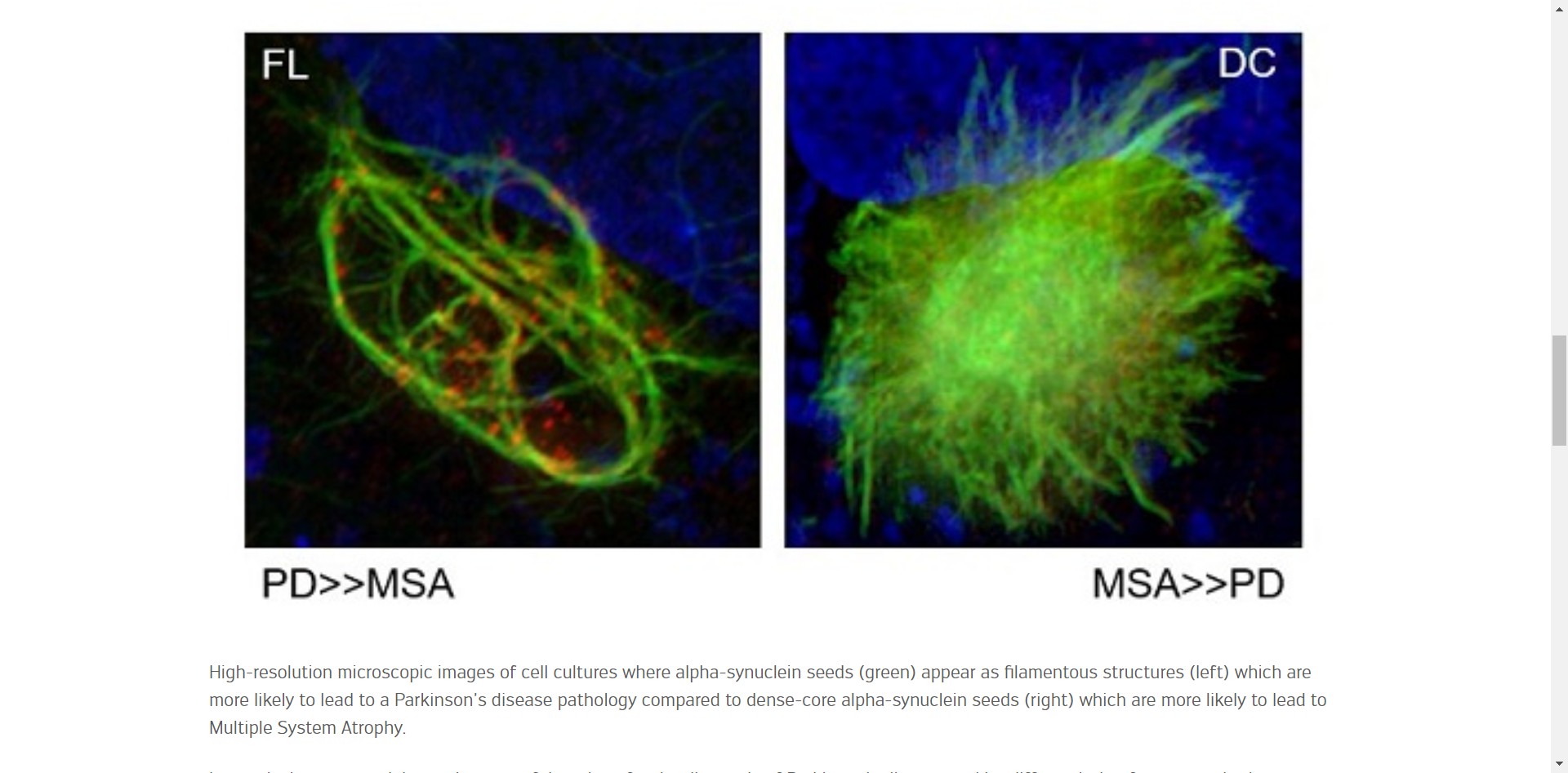
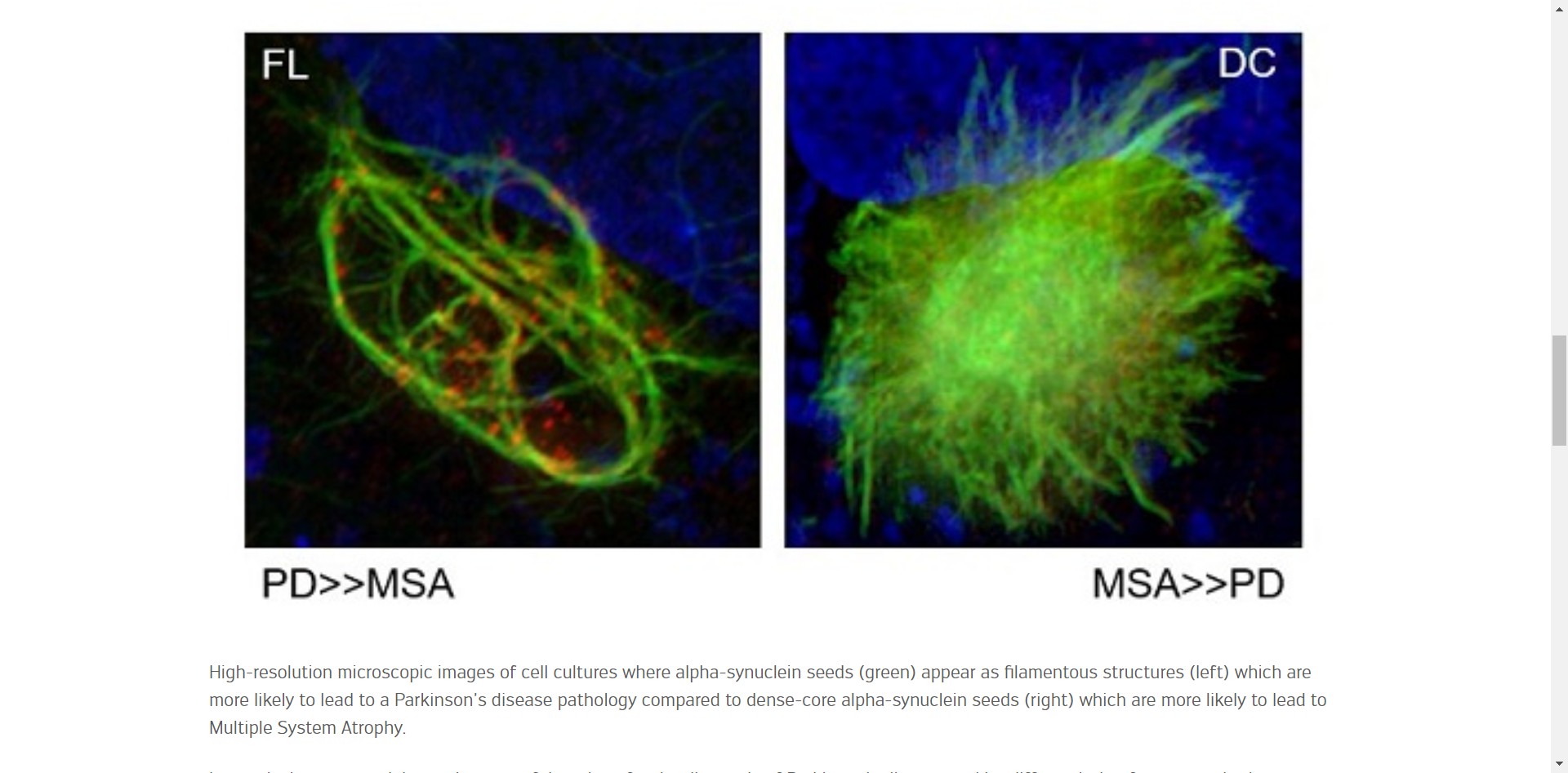
Here we can see the difference
between PD and MSA [multiple system atrophy] filamentous structures which was
found to be significant enough for a distinguishing diagnosis.
Says Prof. Nobutaka Hattori, at the
Department of Neurology of Juntendo University and current head of the
Neurodegenerative Disorders Collaboration Laboratory at RIKEN Centre for Brain
Science,
"'Our team has also discovered, for
the first time, that these α-synuclein seeds have structures and properties
characteristic of each disease, suggesting that they shape the pathology of each
synucleinopathy.'"
https://www.uni.lu/en/news/ground-breaking-discovery-for-diagnosing-neurodegenerative-diseases/
[2983]
How many person years have been lost
to alpha-synucleinopathies due to cannabis prohibition? The Defence believes it
is lots. More than zero.
In a study published in Drug Alcohol
Dependency by Cano, Oh et al (2022)
"Peer-reviewed studies and doctoral
dissertations published in English between 1990 and July 19, 2022 were
identified from PubMed, Web of Science, ProQuest Dissertations & Theses,
PsycINFO, CINAHL, and EconLit. Eligible studies examined at least one
county-level predictor of drug overdose mortality in US counties."
and
"Of 56 studies included, 42.9% were
subnational, and 53.6% were limited to opioid overdose. In multiple studies,
measures related to opioid prescribing, illness/disability, economic distress,
mining employment, incarceration, family distress, and single-parent families
were positively associated with drug overdose mortality outcomes, while measures
related to cannabis dispensaries, substance use treatment, social capital, and
family households were negatively associated with drug overdose mortality
outcomes."
https://www.sciencedirect.com/science/article/abs/pii/S0376871622004513?via%3Dihub
[1823]
“Patients undergoing primary THA
(total hip arthroplasty) or TKA (total knee arthroplasty) with minimum 6-month
follow-up who self-reported cannabis use were retrospectively reviewed. A total
of 210 patients (128 TKAs and 82 THAs) were matched by age; gender; type of
arthroplasty. … Self-reported perioperative cannabis use appeared to
significantly reduce the number of patients that persistently used opioids
greater than 90 days after TJA from 9.5% to 1.4%. [P<.001]”
With cannabis, three patients instead
of 20 showed persistent opioid use.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9493281/ [1824]
In "Use of Cannabis for Harm
Reduction Among People at High Risk for Overdose in Vancouver, Canada
(2016–2018)" Mok et al (2021) report that it's a common strategy for people
trying to recover:
"We drew data about recent cannabis
use and intentions from 3 prospective cohort studies of marginalized people who
use drugs based in Vancouver, Canada, from June 2016 to May 2018. The primary
outcome was “use of cannabis for harm reduction,” defined as using cannabis for
substitution for licit or illicit substances such as heroin or other opioids,
cocaine, methamphetamine, or alcohol; treating withdrawal; or coming down off
other drugs.
"Results. Approximately 1 in 4
participants reported using cannabis for harm reduction at least once during the
study period. The most frequent reasons included substituting for stimulants
(50%) and substituting for illicit opioids (31%)."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8033988/ [3149]
Another meth study "Cannabidiol mechanism of action on modulating extinction and
reinstatement of methamphetamine-seeking behavior: Targeting D2-like dopamine
receptors in the hippocampus" by Omidiani et al (2025):
"Multiple lines of evidence suggest that CBD exerts its effects by modulating
the mesocorticolimbic dopamine system. D2-like receptors in the CA1 region of
the hippocampus play a significant role in relaying memory and emotional signals
related to the processing of drug-related cues. Therefore, this study aims to
investigate the role of CA1 D2-like receptors in mediating the effects of CBD on
METH-seeking behavior during extinction and reinstatement in the conditioned
place preference (CPP) model. For this purpose, rats were administered various
doses of Sulpiride (0.25,1, or 4 μg/0.5 μl) as a D2-like receptor antagonist
before intracerebroventricular (ICV) injection of CBD (10 μg/5 μl) during a
10-day extinction period. Additionally, a separate group of rats received
Sulpiride (0.25,1, or 4 μg/0.5 μl) before a single CBD injection (50 μg/5 μl) on
the reinstatement day. The findings indicated that Sulpiride (1 and 4 μg)
significantly attenuated CBD's acceleration of METH-CPP extinction (p < 0.01 and
p < 0.05, respectively). Moreover, Sulpiride (1 and 4 μg) during the
reinstatement phase notably reversed CBD's preventive effects on the
reinstatement of reward-seeking behavior (p < 0.05 and p < 0.001, respectively).
In summary, these results suggest that CBD's ability to shorten the extinction
period and suppress METH reinstatement is partially mediated through
interactions with D2-like dopamine receptors in the CA1 region of the
hippocampus. These findings offering insight into more precise and effective
interventions for METH use disorder."
https://www.sciencedirect.com/science/article/abs/pii/S0022395625004091
[5402]
Danesh et al (2025) conclude that "D1-like dopamine receptors in the dentate
gyrus mediate cannabidiol's facilitation of extinction and prevention of
reinstatement in methamphetamine-induced conditioned place preference":
"Methamphetamine (METH) is a highly addictive psychostimulant, and despite its
widespread abuse, there are no FDA-approved treatments for METH use disorder
(MUD). Cannabidiol (CBD), a non-psychoactive cannabinoid, has shown promise in
reducing behaviors linked to psychostimulant use, including METH. However, the
underlying neurobiological mechanisms remain unclear. Emerging evidence suggests
that CBD may act on the dopamine system to influence drug-seeking behavior.
D1-like dopamine receptors (D1Rs) in the hippocampus (HPC) are involved in
memory processes related to rewards, which may contribute to CBD's effects. This
study examined whether D1Rs in the dentate gyrus (DG) region of the HPC play a
role in CBD's modulation of METH-induced conditioned place preference (CPP)
during extinction and reinstatement. Adult male Wistar rats received the D1Rs
antagonist SCH23390 (0.25, 1, and 4 μg/0.5 μl saline) into the DG region before
intracerebroventricular injection of CBD (10 and 50 μg/5 μl of 12 % DMSO).
Results show that the highest dose of SCH23390 (4 μg) significantly blocked
CBD's ability to enhance extinction of METH-CPP. Moreover, SCH23390 (1 and 4 μg)
reversed CBD's prevention of reinstatement of METH-CPP. These findings suggest
that D1Rs in the DG region are involved in mediating CBD's effects and offer
insights into its therapeutic potential for MUD."
https://www.sciencedirect.com/science/article/abs/pii/S0091305725001418
[5403]
Balu et al (2021) report:
"Overall, the average change in
prescribed opioid use was found to be -12.3 morphine milligram equivalent (MME)
units when including all individuals (p < 0.00001)."
They break it down.
“In this study, we examined
individuals who were provided with legal; medical cannabis certifications in the
state of Delaware between June 2018 and October 2019 and were concurrently being
treated with opioid medications for chronic pain at a private pain management
practice. … For non-outlier individuals with positive baseline opioid use before
receiving medical marijuana certification (n=63), the average percent change in
opioid use was found to be -31.3 percent. Examining subgroups based upon pain
location, individuals with low back pain (n=58) displayed a 29.4 percent
decrease in MME [morphine milligram equivalent] units, while individuals with
neck pain (n=27) were observed to have a 41.5 percent decrease in opioid use.
Similarly, individuals with knee pain (n=14) reduced their opioid use by 32.6
percent. … Since the underlying pathology and their source of pain in the
individuals was unlikely to significantly change during the period examined,
medical marijuana use could have played a large role in allowing the individuals
to decrease their opioid use."
https://www.cureus.com/articles/77114-medical-cannabis-certification-is-associated-with-decreased-opiate-use-in-patients-with-chronic-pain-a-retrospective-cohort-study-in-delaware
[1825]
More than a quarter of U.S. adults
suffering from chronic pain have turned to using cannabis to manage their
discomfort, according to a study published in JAMA Open Network.
Researchers at Michigan Medicine
surveyed 1,661 adults last spring with chronic pain who lived in one of the 36
states with active medical cannabis programs and Washington, D.C.
About 26 percent of survey
participants reported using cannabis within the past year to manage pain, Bicket
et al found. Moreover:
"More than half of adults who used
cannabis to manage their chronic pain reported that use of cannabis led them to
decrease use of prescription opioid, prescription nonopioid, and over-thecounter
pain medications, and less than 1% reported that use of cannabis increased their
use of these medications (Figure 1). Fewer than half of respondents reported
that cannabis use changed their use of nonpharmacologic pain treatments. Among
adults with chronic pain in this study, 38.7% reported that their used of
cannabis led to decreased use of physical therapy (5.9% reported it led to
increased use), 19.1% reported it led to decreased use of meditation (23.7%
reported it led to increased use), and 26.0% reported it led to decreased used
of cognitive behavioral therapy (17.1% reported it led to increased use) (Figure
2)."
https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2800119/bicket_2023_ld_220293_1671719838.02096.pdf
[2011]
"Δ8-Tetrahydrocannabivarin has potent
anti-nicotine effects in several rodent models of nicotine dependence" revealed
Xi et al in 2019:
"Both types of cannabinoid
receptors—CB1 and CB2— regulate brain functions relating to addictive
drug-induced reward and relapse. CB1 receptor antagonists and CB2 receptor
agonists have anti-addiction efficacy, in animal models, against a broad range
of addictive drugs. Δ9-Tetrahydrocannabivarin (Δ9-THCV)—a cannabis
constituent—acts as a CB1 antagonist and a CB2 agonist.
Δ8-Tetrahydrocannabivarin (Δ8-THCV) is a Δ9-THCV analogue with similar combined
CB1 antagonist/CB2 agonist properties.
"Experimental Approach: We tested
Δ8-THCV in seven different rodent models relevant to nicotine
dependence—nicotine self-administration, cue-triggered nicotine-seeking
behaviour following forced abstinence, nicotine-triggered reinstatement of
nicotine-seeking behaviour, acquisition of nicotine-induced conditioned place
preference, anxiety-like behaviour induced by nicotine withdrawal, somatic
withdrawal signs induced by nicotine withdrawal, and hyperalgesia induced by
nicotine withdrawal.
"Key Results: Δ8-THCV significantly
attenuated intravenous nicotine self-administration and both cue‐induced and
nicotine-induced relapse to nicotine-seeking behaviour in rats. Δ8-THCV also
significantly attenuated nicotine-induced conditioned place preference and
nicotine withdrawal in mice."
and
"In summary, most studies on animal
models for substance use disorders reported some beneficial effects for the
cannabinoids under investigation, except for CBDA (see Fig. 3). Δ8-THCV showed
anti-nicotine-dependence properties, while CBN, Δ8-THC, and 11-OH-Δ8-THC
appeared to reduce morphine-withdrawal symptoms. Δ8-THC also seemed to have some
capacity to inhibit the reinstatement of METH-seeking behavior. CBDA was not
effective in reducing METH-induced or cocaine-seeking behaviors."
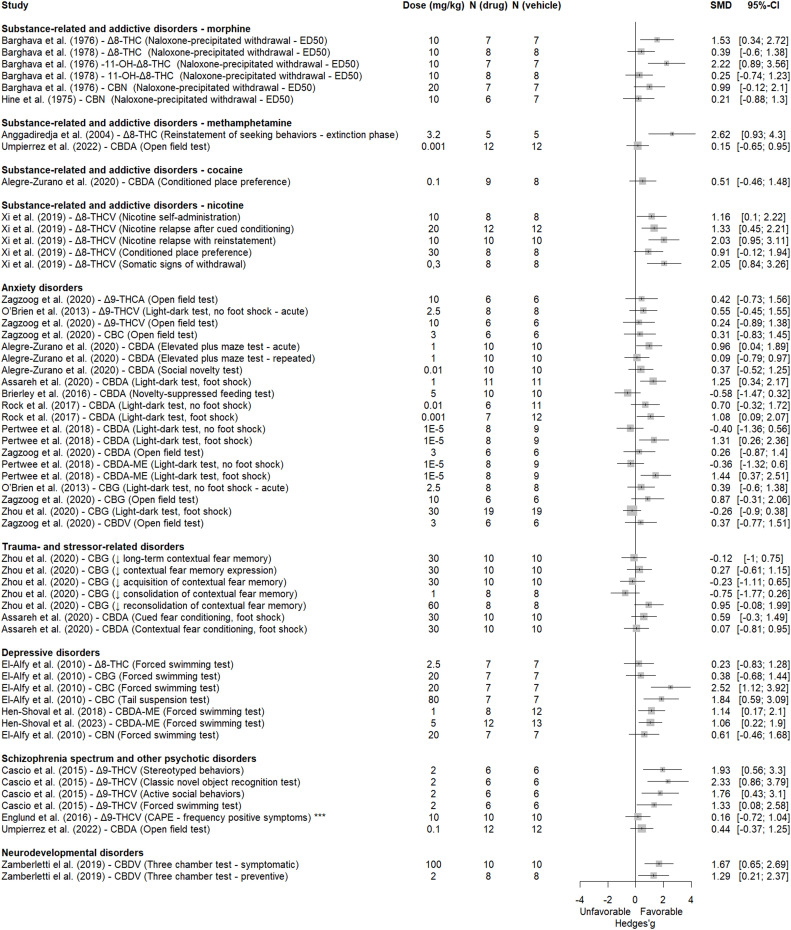
https://bpspubs.onlinelibrary.wiley.com/doi/pdfdirect/10.1111/bph.14844[3808]
Kitchen et al (2025) examined "Cannabis use
and illicit opioid cessation among people who use drugs living with chronic
pain":
"Between June 2014 and May 2022, 2340 PWUD were initially recruited and of those
1242 PWUD reported chronic pain, use of unregulated opioids and completed at
least two follow-up visits. Of these 1242 participants, 764 experienced a
cessation event over 1038.2 person-years resulting in a cessation rate of 28.5
per 100 person-years (95% confidence interval [CI] 25.4–31.9). Daily cannabis
use was positively associated with opioid cessation (adjusted hazard ratio 1.40,
95% CI 1.08–1.81; p = 0.011). In the sex-stratified sub-analyses, daily cannabis
use was significantly associated with increased rates of opioid cessation among
males (adjusted hazard ratio 1.50, 95% CI 1.09–2.08; p = 0.014)."
https://onlinelibrary.wiley.com/doi/abs/10.1111/dar.14014 [4794]
"Efficacy of cannabidiol alone or in combination with Δ-9-tetrahydrocannabinol
for the management of substance use disorders: An umbrella review of the
evidence" from Bertrand Redonnet et al (2025)
"...searched PubMed, Web of Science and Epistemonikos databases for SRs, with or
without a meta-analysis, of randomized controlled trials focusing on
interventions dispensing CBD, alone or in combination with THC, to treat SUDs,
published from 1 January 2000 to 15 October 2024.
The results supported combined THC and CBD:
"22 SRs were included, 5 of which performed a meta-analysis. We found mixed
evidence regarding the efficacy of CBD to manage and treat SUDs. Findings were
interpreted in light of the quality of the SRs. Nabiximols, which contains CBD
and THC, demonstrated positive effects on cannabis withdrawal and craving
symptoms. Evidence supporting the efficacy of CBD is limited and inconclusive
for abstinence, reduction or cessation of use of cannabis, tobacco, alcohol,
opiates and other psychoactive substances.
"Conclusion
Cannabidiol (CBD) monotherapy does not appear to be efficacious for treatment of
substance use disorders. CBD primarily exhibits effects on cannabis withdrawal
and craving when combined with Δ-9-tetrahydrocannabinol (THC). Existing data on
the efficacy of CBD alone with regard to other outcomes related to substance use
disorders are limited."
https://onlinelibrary.wiley.com/doi/10.1111/add.16745 [4755]
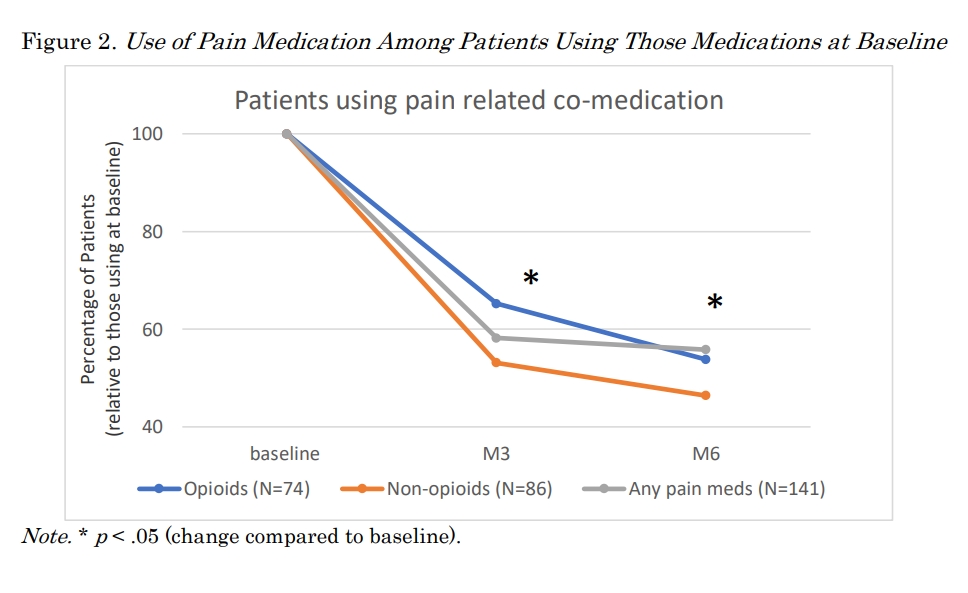
https://publications.sciences.ucf.edu/cannabis/index.php/Cannabis/article/download/239/169
[4767]
Several descriptive commentaries from opoid users fighting addiction are
featured in Ganesh et al (2024) "'Smoking weed it gets you over the hump':
Cannabis co-use as a facilitator of decreased opioid use among people who inject
drugs in Los Angeles, California" including this one:
"Participants also described using cannabis to mitigate opioid cravings after
they had stopped regular use and were no longer experiencing withdrawal
symptoms. This person reported that it helped them to 'get over the hump' of
craving opioids and continue not to use.
"'I was really trying to get off of opiates and using weed, really helps to not
have the first urge to use opiates. When you're addicted and you have a habit,
then you have to use opiates. But when you don't have a habit and you're not
getting sick from it every day, when you're smoking weed it gets you over the
hump and that urge to get high for the first time. And that's what's so special
out [sic] weed.' (5115 – 26, Male, Housed)"
https://www.sciencedirect.com/science/article/pii/S2772724624000416 [5063]
Looking at "Recreational Cannabis Laws and Fills of Pain Prescriptions in the
Privately Insured" Steuart et al (2025) found no good cheer for the
manufacturers and distributors of opioids:
"Objective: Almost half of U.S. states have passed recreational cannabis laws as
of May 2024. While considerable evidence to date indicates cannabis may be a
substitute for prescription opioids in the treatment of pain, it remains unclear
if patients are treating pain with cannabis alone or concomitantly with other
medications.Method: Using data from a national sample of commercially insured
adults, we examine the effect of recreational cannabis legalization (through two
sequential policies) on prescribing of opioids, NSAIDS, and other pain
medications by implementing synthetic control estimations and constructing
case-study level counterfactuals for the years 2007-2020. Results: Overall, we
find recreational cannabis legalization is associated with a decrease in opioid
fills among commercially insured adults in the U.S., and we find evidence of a
compositional change in prescriptions of pain medications more broadly.
Specifically, we find marginally significant increases in prescribing of
non-opioid pain medications after recreational cannabis becomes legal in some
states. Once recreational cannabis dispensaries open, we find statistically
significant decreases in the rate of opioid prescriptions (13% reduction from
baseline, p<.05) and marginally significant decreases in the average daily
supply of opioids (6.3% decrease, p<.10) and number of opioid prescriptions per
patient (3.5% decrease, p<.10). Conclusions: These results suggest that
substitution of cannabis for traditional pain medications increases as the
availability of recreational cannabis increases. There appears to be a small
shift once recreational cannabis becomes legal, but we see stronger results once
users can purchase cannabis at recreational dispensaries.The decrease in opioids
and marginal increase in non-opioid pain medication may reflect patients
substituting opioids with cannabis and non-opioid pain medications, either
separately or concomitantly. Reductions in opioid prescription fills stemming
from recreational cannabis legalization may prevent exposure to opioids in
patients with pain and lead to decreases in the number of new opioid users,
rates of opioid use disorder, and related harms."
https://publications.sciences.ucf.edu/cannabis/index.php/Cannabis/article/view/268/181
[5073]
Carey et al (2025) created some junkie
monkeys to test the "Effects of Δ9-tetrahydrocannabinol (THC), cannabidiol
(CBD), and THC:CBD mixtures on behavioral and physiological signs of morphine
withdrawal in rhesus monkeys":
"Monkeys received escalating doses of morphine up to 3.2 mg/kg twice daily.
After at least 2 weeks of morphine treatment, saline was substituted for
morphine for 2 days. Behavioral and physiological signs of opioid withdrawal,
including blood pressure, heart rate, body temperature, and activity were
measured before and after administration of THC (0.32–1.0 mg/kg), CBD (10–17.8
mg/kg), mixtures of THC (0.32 mg/kg) and CBD (10–17.8 mg/kg), lofexidine
(0.032–0.32 mg/kg), or vehicle. Discontinuing morphine treatment markedly
increased unusual tongue movements, a characteristic behavioral sign of opioid
withdrawal in monkeys, and all physiological signs. The largest THC dose (1.0
mg/kg) decreased unusual tongue movements and heart rate, and the largest
lofexidine dose (0.32 mg/kg) decreased unusual tongue movements, blood pressure,
heart rate, and activity. CBD alone or with THC had no significant effect. These
data demonstrate that THC attenuates some signs of opioid withdrawal; however,
THC was not more effective than the currently available medication lofexidine."
https://www.sciencedirect.com/science/article/abs/pii/S0022356525398848
[5326]
In "Cannabis Use, Problem-Gambling
Severity, and Psychiatric Disorders: Data from the National Epidemiological
Survey on Alcohol and Related Conditions" (2019) Hammond et al
"... examined data from the first
wave (2001–2002) of the National Epidemiological Survey on Alcohol and Related
Conditions (NESARC), a large, national survey of non-institutionalized U.S.
adults, to examine relationships between problem-gambling severity and
psychopathology in individuals with and without cannabis use. At the time of
data collection of the first wave of the NESARC, medical cannabis use had been
legalized in eight states; however, its recreational or non-medical use had not
been legalized in any state. In addition, prevalence estimates of past-year use
during this time period has ranged from 4.1% (Hasin et al., 2015) to 11%
(Azofeifa, Mattson, Schauer, McAfee, Grant, & Lyerla, 2016). "In all cases,
associations between problem-gambling severity and psychopathologies were weaker
among the lifetime-cannabis-using group as compared to the never-using group..
Cannabis use moderates the relationships between problem-gambling severity and
psychiatric disorders, with cannabis use appearing to account for some of the
variance in the associations between greater problem-gambling severity and
specific forms of psychopathology."
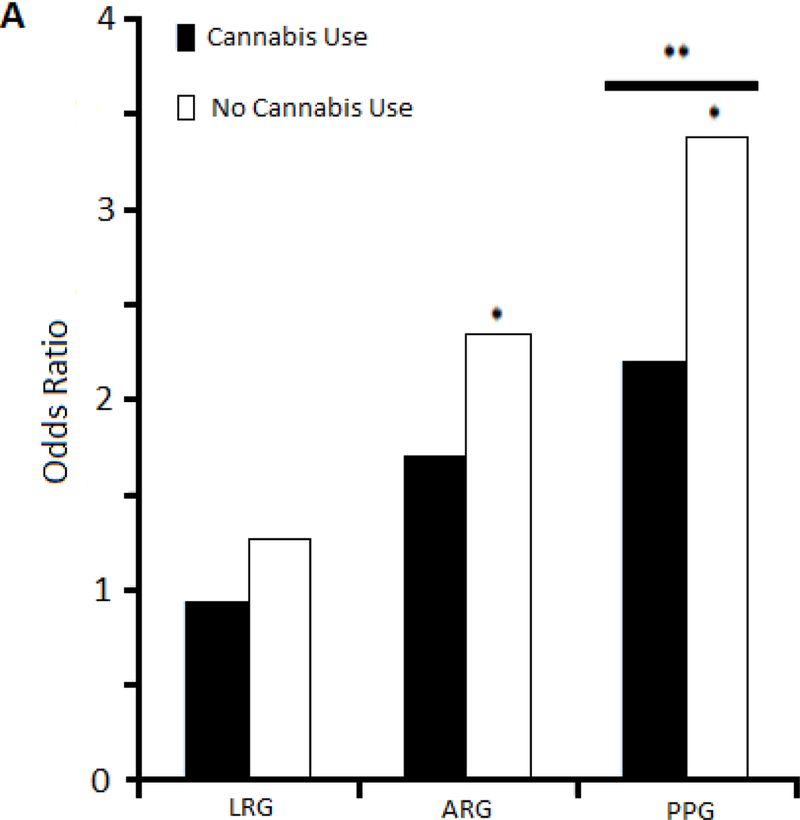
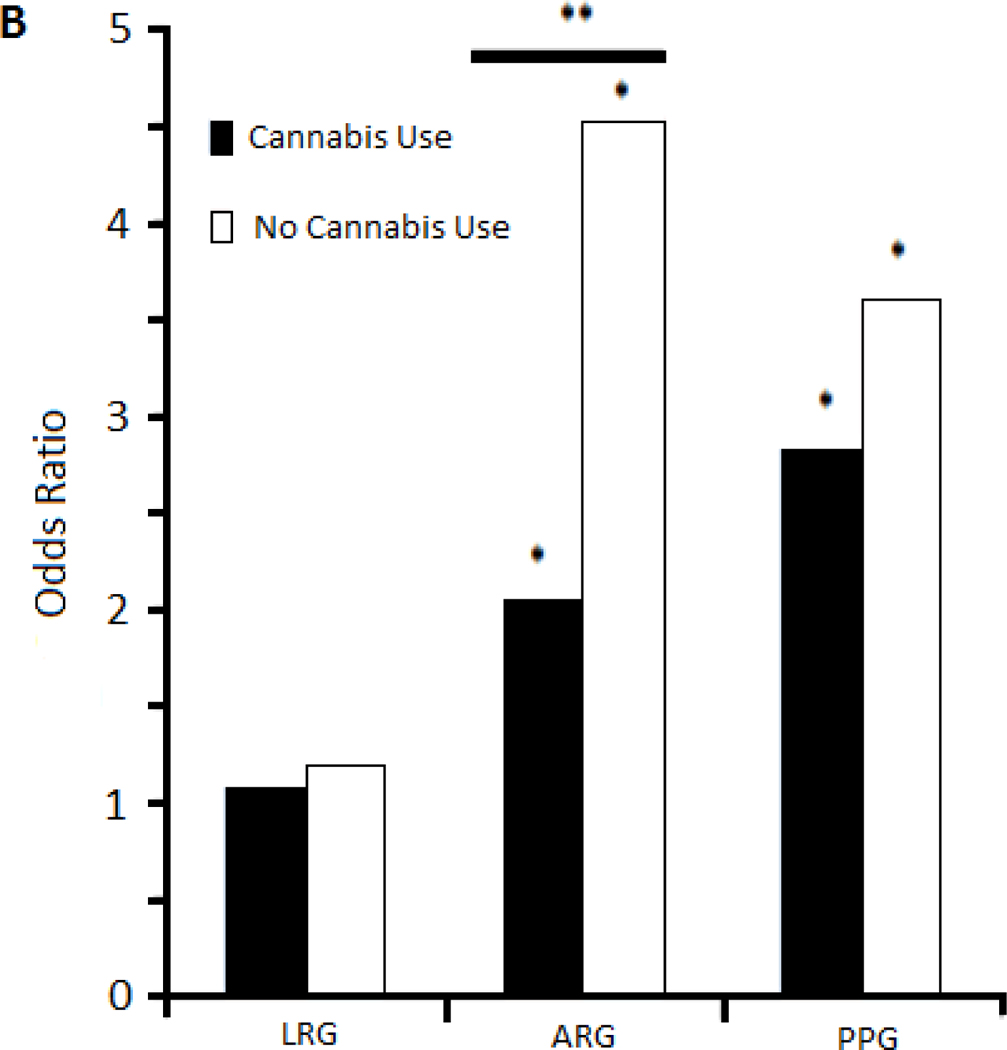
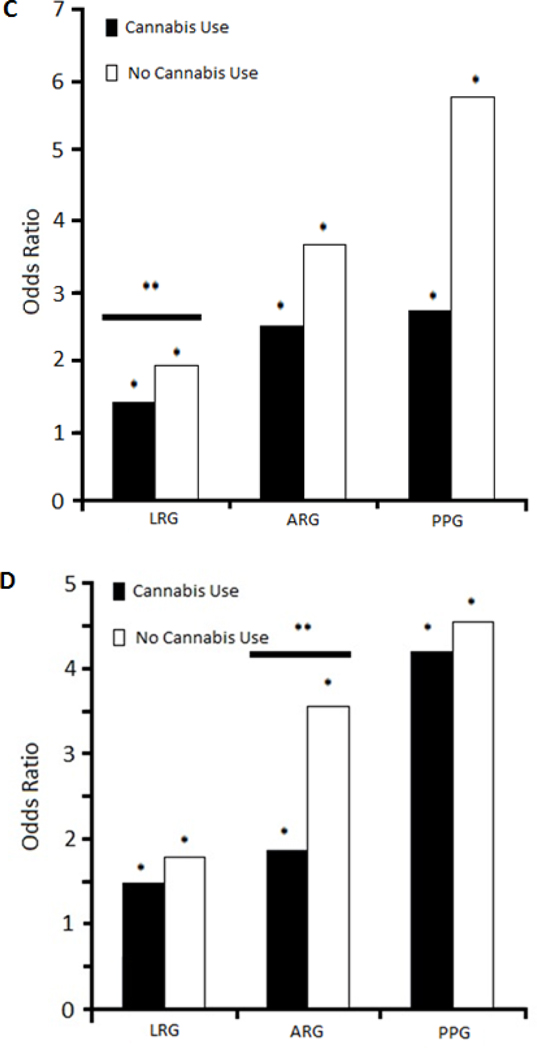
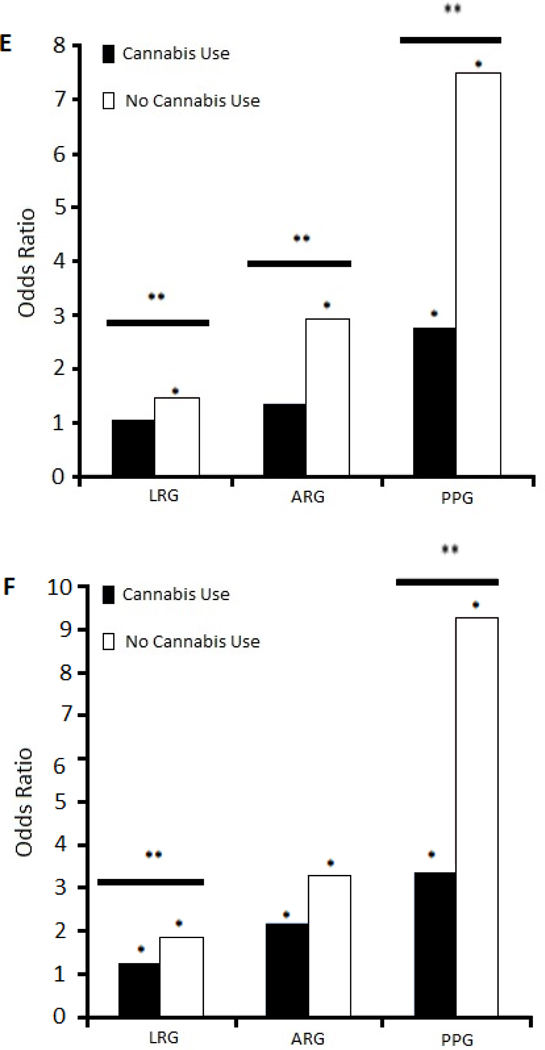
"Associations between
problem-gambling severity and psychopathology among lifetime-cannabis-using and
never-using groups. Figures compare odds ratios for specific disorders in
association with low-risk gambling (LRG), at-risk gambling (ARG), and
problem/pathological gambling (PPG), using of non-gambling/low frequency
gambling as a reference group. Specific disorders are those as follows: A.
Interactions with cannabis use in the associations between major depression and
problem-gambling severity. B. Interactions with cannabis use in the associations
between panic disorder and problem-gambling severity. C. Interactions with
cannabis use in the associations between alcohol abuse/dependence and
problem-gambling severity. D. Interactions with cannabis use in the associations
between nicotine dependence and problem-gambling severity. E. Interactions with
cannabis use in the associations between cluster A personality disorder and
gambling severity. F. Interactions with cannabis use in the associations between
cluster B personality disorders and problem-gambling severity. * Indicates
statistically significant odds ratios at p<0.05. ** Indicates statistically
significant interactions at p<0.05."
and
"Furthermore, cannabis-use status
moderated the relationships problem-gambling severity and specific psychiatric
disorders including major depression, panic disorder, alcohol-use disorders,
nicotine dependence, cluster A PDs (especially paranoid PD), and cluster B PDs
(especially antisocial PD)."
However Dr Hammond, who has
"...received support from the
American Psychiatric Association Child & Adolescent Fellowship, an unrestricted
education grant supported by Shire Pharmaceuticals and the American Academy of
Child & Adolescent Psychiatry Pilot Research Award for Junior Investigators
supported by Lilly USA, LLC. Dr. Marc Potenza has received financial support or
compensation for the following: Dr. Potenza has consulted for and advised Shire,
INSYS, RiverMend Health, Opiant/Lakelight Therapeutics, and Jazz
Pharmaceuticals; has received unrestricted research support from Mohegan Sun
Casino and grant support from the National Center for Responsible Gaming"
...tries to highlight cannabis in
problem gambling, his own Figure 1 tells the real story. Even under prohibition
conditions, it was another blow for NECUD/SPUK sufferers, who were worse at
gambling and at being crazy too.
I've used my incredible graphics
skills to show how the anti-cannabis woowoo is favoured by the layout of the
histograms in Figure 1.
Please compare
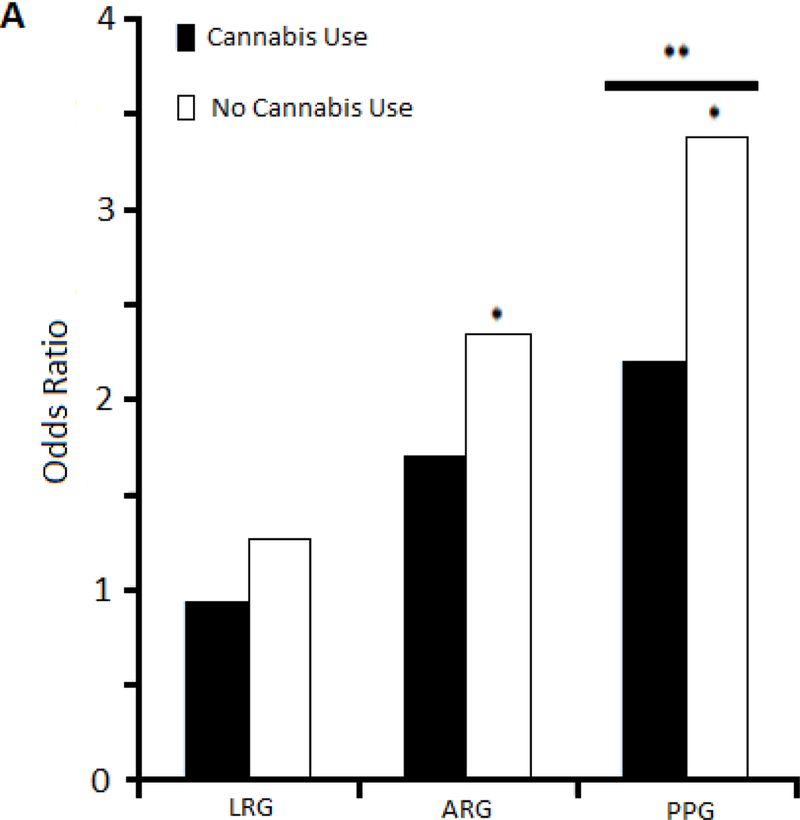
...which charts interactions with
cannabis use in the associations between major depression and problem-gambling
severity for low-risk gambling (LRG), at-risk gambling (ARG), and
problem/pathological gambling (PPG groups), with
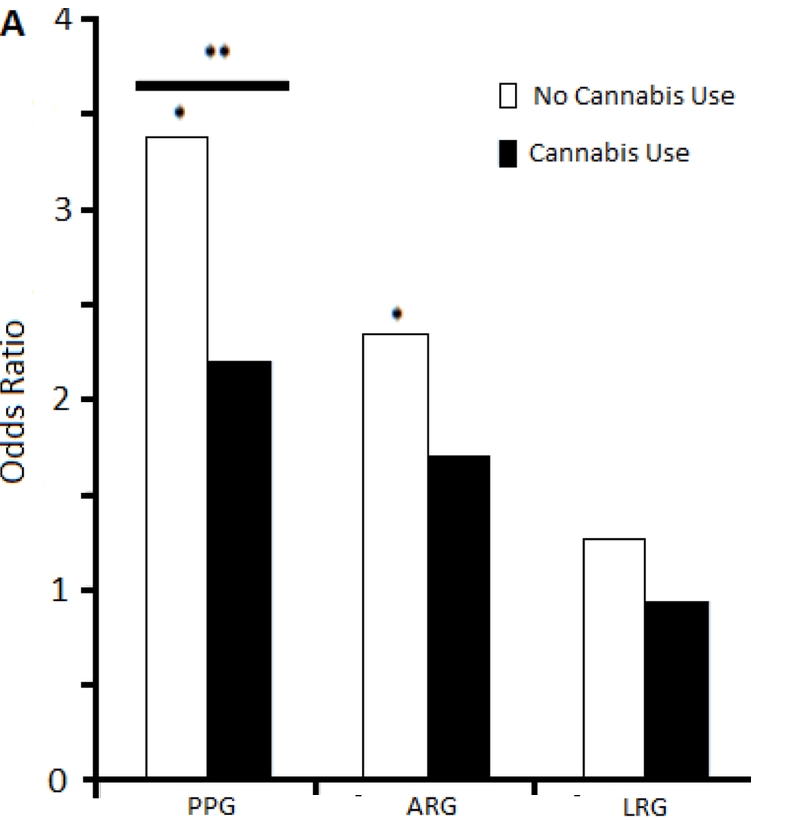
...a left to right mirror image of
1A. You can see cannabis looks much better now, and we have begun with the most
serious problem gamblers and worked our way downwards. I have not done mirror
images for charts B-F, I'm sure the Court can imagine that for itself.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6933114 [2711]
Another survey, published in JAMA
Psychiatry by Grubbs and Kraus in 2024, found a relationship between problem
drinking and problem gambling:
"A total of 4363 respondents were
included (51.4% men, 46.4% women, and 2.2% nonbinary or other; mean [SD] age,
49.6 [16.2] years) (Table 1). The national census-matched survey consisted of
2806 participants (mean [SD] age, 48.9 [17.2] years; 1365 [48.6%] men and 1441
[51.4%] women; response rate, 2806 of 3203 [87.6%]). The oversample of sports
gamblers consisted of 1557 participants (mean [SD] age, 41.7 [15.3] years; 1043
[67.0%] men and 514 [33.0%] women; response rate, 1557 of 1978 [78.7%]), of whom
1474 reported past year sports betting. Additionally, in the national sample,
338 respondents (12.0%) indicated they had gambled on sports in the past 12
months, resulting in a total of 1812 sports gamblers (Table 1). Sports gamblers
were disproportionally likely to be men and younger. In these combined samples,
3267 respondents (74.9%) reported past year alcohol use. Sports wagerers were
disproportionately more likely to report binge drinking at monthly or greater
frequency over the past 12 months and were also disproportionately less likely
to report no binge drinking episodes in the past 12 months (Table 1).
Multinomial logistic regressions adjusted for age and race and ethnicity showed
that sports gamblers were substantially more likely to report higher levels of
binge drinking (Table 2), suggesting that elevated risky drinking episodes among
sports gamblers are not due to demographic differences."
https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2816784/grubbs_2024_ld_240031_1710953595.81812.pdf
[3483]
In view of the foregoing, we should
not be surprised if "Expectancy of impairment attenuates marijuana-induced risk
taking" (2017):
"Participants (N=136) were regular
marijuana users. A balanced placebo design (BPD) was used crossing marijuana
administration (i.e., 0% Tetrahydrocannabinol (THC) vs. 2.8% THC) with stimulus
expectancy (i.e., Told Placebo vs. Told THC). Marijuana outcome expectancies
were measured by self-report and dependent measures including a number of
behavioral impulsivity tasks and the balloon analogue risk task (BART).
Results—Among participants who received THC, higher expectancies for
cognitive-behavioral impairment (CBI) were related to lower risk-taking on the
BART. Among those who received placebo, there was no association between CBI
expectancies and BART performance. CBI expectancies did not moderate drug effect
on the BART and drug or stimulus expectancy effects on impulsivity measures."
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC5796549&blobtype=pdf
[2712]
"Treating alcoholism by cannabis substitution creates a different doctor-patient
relationship," says Mikuriya.
"Patients seek out the physician to confer legitimacy on what they are doing or
are about to do. My most important service is to end their criminal status,
Aeschalapian protection from the criminal justice system, which often brings an
expression of relief. An alliance is created that promotes candor and trust. The
physician is permitted to act as a coach or an enabler in a positive sense."
[3822]
Summarising the criteria for any substitution "treatment"...
"1. It should reduce alcohol use and related harms.
"2. It should ideally be free of harms, or at least less harmful than alcohol.
"3. Misuse should be less than that of alcohol.
"4. It should be shown that it can substitute for alcohol and not be used along
with alcohol.
"5. It should be safer in overdose than alcohol.
"6. It should ideally not potentiate the effects of alcohol especially if either
drug is taken in overdose.
"7. It should offer significant health economic benefits."
...Chick and Nutt (2012) found six criteria wholly satisfied by cannabis, while
one (number 6) was partially satisfied, due to disagreement on whether it
potentiates alcohol. The answer to that is, only if you drink alcohol. For
details see Subbaraman's Table 1.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3992908/ [3823]
Cannabis legalisation in Slovenia can be expected to reduce morbidity, mortality
and costs related to tobacco use. According to a survey of 9003 subjects by
Pravosud et al (2024)
"In this longitudinal study, a web-based survey was administered to a nationally
representative, population-based panel of US adults in 2017, 2020, and 2021. We
used weighted unadjusted binomial logistic GEE models to assess changes in
prevalence of cannabis, tobacco/nicotine use and co-use and weighted, adjusted
binary logistic GEE models to assess associations of cannabis legalization with
cannabis, tobacco/nicotine use and co-use."
"Between 2017 and 2021 current cannabis use increased +3.3 % and was higher in
states with medical and recreational cannabis.
"Recreational cannabis legalization increased the odds of current cannabis use
by 1.13 times above the effect of medical legalization.
"Current tobacco use declined −1.9 %, but this change was not associated with
legalization."
https://www.sciencedirect.com/science/article/pii/S0955395924003025?via%3Dihub
[4810]
----------------------------------------------------------------------------
The Englishman stands
for the rights of everyone disadvantaged, discriminated against, persecuted, and
prosecuted on the false or absent bases of prohibition, and also believes the
victims of these officially-sanctioned prejudices have been appallingly treated
and should be pardoned and compensated.
The Englishman requests the return of his
CaPs
and other rightful property, for whose distraint Slovenia has proffered no
credible excuse or cause.
The Benedictions represent both empirical entities as well as beliefs. Beliefs
which the Defence evidence shows may be reasonably and earnestly held about the
positive benefits of CaPs at the population level, in which the good
overwhelmingly outweighs the bad. Below, the latest version of this dynamic
list.
THE BENEDICTIONS
REFERENCES
TIMELINE OF DRUG LAW v. SCIENCE