PTSD BIOMARKERS
"In 1980, the American Psychiatric Association (APA)
added PTSD to the third edition of its Diagnostic and Statistical Manual of
Mental Disorders (DSM-III) nosologic classification scheme. Although
controversial when first introduced, the PTSD diagnosis has filled an important
gap in psychiatric theory and practice.
https://www.ptsd.va.gov/professional/treat/essentials/history_ptsd.asp#:~:text=In%201980%2C%20the%20American%20Psychiatric,in%20psychiatric%20theory%20and%20practice [2132]
Accounts of PTSD-like symptoms can be found in the
Epic of Gilgamesh, the writings of Herodotus and Hippocrates, and in the Indian
epic poem Ramayana.
Terms used of the years included shell shock,
soldier’s heart, irritable heart, Da Costa's syndrome, combat fatigue or war
neurosis. And for a a couple of centuries "nostalgia" - not its present meaning:
"In the late 1600s, Swiss physician Dr. Johannes Hofer
coined the term 'nostalgia' to describe Swiss soldiers who suffered from despair
and homesickness, as well as classic PTSD symptoms like sleeplessness and
anxiety. Around the same time, German, French and Spanish doctors described
similar illnesses in their military patients.
"In 1761, Austrian physician Josef Leopold Auenbrugger
wrote about nostalgia in trauma-stricken soldiers in his book Inventum Novum.
The soldiers, he reported, became listless and solitary, among other things, and
efforts could do little to help them out of their torpor.
"PTSD in the Civil War
Nostalgia was a phenomenon noted throughout Europe and
the 'disease' reached American soil during the U.S. Civil War (1861–1865). In
fact, nostalgia became a common medical diagnosis that spread throughout camps.
But some military doctors viewed the illness as a sign of weakness and one that
only affected men with a 'feeble will'—and public ridicule was sometimes the
recommended 'cure' for nostalgia."
https://www.history.com/topics/inventions/history-of-ptsd-and-shell-shock
[2133]
Shivitti is a sort of case study, The author was
sufficiently impressed by his psychedelic outcome that he wrote a book about it:
"An autobiographical record of one Holocaust
survivor’s triumph over concentration camp syndrome with a regimen of
professionally administered LSD.
"Imprisoned in Auschwitz for two years, having eluded
death by the narrowest of margins, the man known as Ka-tzetnik 135633 survived
the Holocaust to discover that survival alone would not end his torment. For
over 30 years, through nightly dreams of terrifying intensity, the writer
remained captive to the horrors of Auschwitz. Finally in 1976 he sought help
from Professor Jan Bastiaans, the Dutch psychiatrist who first recognized
Concentration Camp Syndrome and successfully treated camp survivors with a
therapy involving doses of LSD. Shivitti is a memoir of that experience."
https://maps.org/product/shivitti-a-vision/ [3548]
Trauma author Dr David Healy charts the course of its
treatment from the Civil War, before and after Freudianism, to the post-Vietnam
intervention of the DSM and its gradual generalisation to to the traumas common
in life, to today. Slovenia's own slant on all of this is an uncooked omlette.
"The word shellshock essentially rebranded hysteria,
which up till WW I had been a disorder of women and people with weaker
constitutions. A new name was needed because in WW I officers, no less than the
working class men in trenches, were badly affected. Women in contrast were
becoming surgeons and running hospitals back at home. The social order was
shaken up. There was an uptick of births linked to WW I but not as dramatic as
the increase 30 years later.
"Shellshock helped make Freud’s reputation.
Paradoxically, Freud came to the fore not because he believed trauma was a
factor causing nervous problems but because his position was that trauma,
whether War or Sexual Abuse in childhood, was irrelevant. People broke down in
War or in Life, because they had pre-existing adjustment difficulties linked to
poor prior management of their libidinous impulses. Current difficulties
(trauma) played into the prior weakness. See Shipwreck in Maastricht.
"This view excuses the powers that be from causing our
nervous breakdowns. It stops us suing governments for drafting us into military
or vaccine wars. It lays a basis for pointing to a pre-existing mendacity of
women when they claim sexual abuse or rape.
"Thinking on these lines was not unique to Freud. It
played a growing part in industrial accidents and ‘mental trauma’ linked to
these accidents in American legal cases from the creation of railroads in the
1850s onwards.
"It shaped how the American military dealt with the
question of military pensions after the Civil War – ultimately creating in the
US what might be called the first single party payer health service anywhere in
the world. It colored how Germany and Britain dealt with Shellshock after WW I.
"For WW II the Americans screened men for
psychological weakness and excluded them. This did nothing to eliminate the
problems. The War and the post War nervous problems entrenched psychoanalytic
thinking in the United States. The Europeans went to War armed with high dose
barbiturates, which helped in many but not all cases.
"Analysis came out of the War strengthened. This led
to claims that it was obvious where the War had come from – the Germans were
maladjusted. Democrat voting psychiatrists, unlike Republican voting doctors in
general, knew what was wrong with Republican politicians like Goldwater and
Reagan – they were latent homosexuals. In an era when Americans put a man on the
moon, the shrinks figured it was within reach to prevent Wars by curing our
neuroses.
"Data on personality profiles showing that German
concentration camp guards were more normal and less psychopathic than the
American G.I.s who liberated the camps did nothing to change minds on this."
...and his analysis comes to a frightening conclusion
about industrialized medicine.
Today we seek biological explanations - to produce
targeted cures.
But PTSD biomarkers remain a topic of some complexity
with little opportunity for access to analyses for ordinary patients.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4520791/ [51]
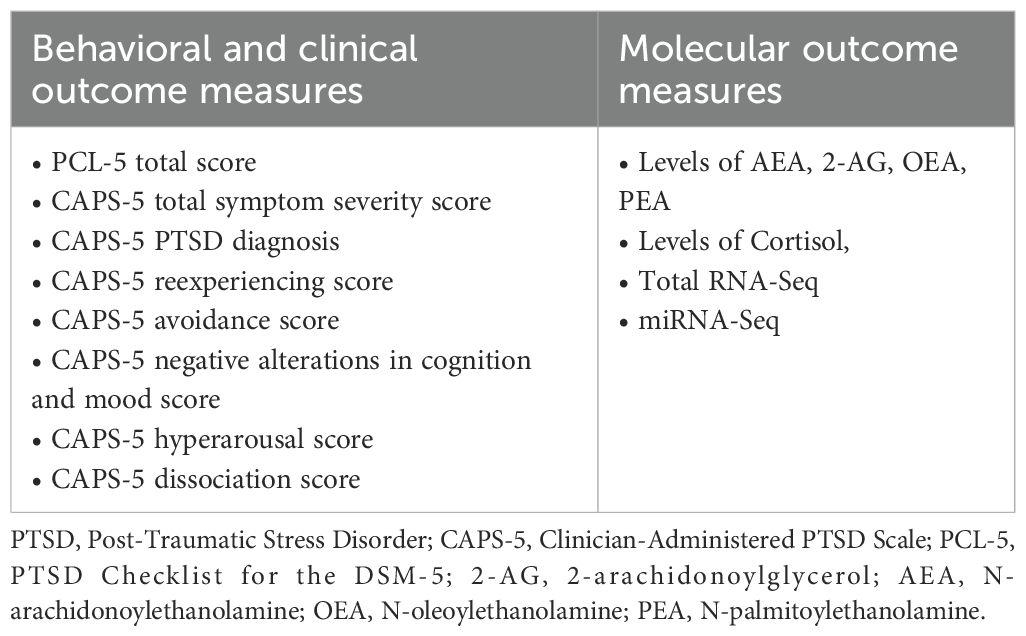
List of potential tests in Table 1
The last biomarker mentioned is lowered
endocannabinoids, and reference 64 refers to
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3870889/ [52]
in which AEA and 2-AG were assayed in addition to
cortisol in survivors of the WTC collapse, so the patients were all exposed to
similar experiences at the same time, increasing its usefulness
"The effect of reduced 2-AG content in PTSD remained
significant after controlling for the stress of exposure to the WTC collapse,
gender, depression and alcohol abuse. There were no significant group
differences for AEA or cortisol levels; however, across the whole sample AEA
levels positively correlated with circulating cortisol, and AEA levels exhibited
a negative relationship with the degree of intrusive symptoms within the PTSD
sample. This report shows that PTSD is associated with a reduction in
circulating levels of the eCB 2-AG. Given the role of 2-AG in the regulation of
the stress response, these data support the hypothesis that deficient eCB
signaling may be a component of the glucocorticoid dysregulation associated with
PTSD. The negative association between AEA levels and intrusive symptoms is
consistent with animal data indicating that reductions in AEA promote retention
of aversive emotional memories."
The ventromedial prefrontal cortex may contribute to
conditioned response inhibition via suppression of the amygdala.
https://www.jneurosci.org/content/jneuro/26/37/9503.full.pdf [148]
Hwang et al (2025) relate how...
"Recent studies have begun to detail the molecular biology of PTSD. However,
given the array of PTSD-perturbed molecular pathways identified so far, it is
implausible that a single cell type is responsible. Here we profile the
molecular responses in over two million nuclei from the dorsolateral prefrontal
cortex of 111 human brains, collected post-mortem from individuals with and
without PTSD and major depressive disorder. We identify neuronal and
non-neuronal cell-type clusters, gene expression changes and transcriptional
regulators, and map the epigenomic regulome of PTSD in a cell-type-specific
manner. Our analysis revealed PTSD-associated gene alterations in inhibitory
neurons, endothelial cells and microglia and uncovered genes and pathways
associated with glucocorticoid signalling, GABAergic transmission and
neuroinflammation."
https://www.nature.com/articles/s41586-025-09083-y [5255]
The locus coeruleus
(LC) is a small, bluish nucleus located in the brainstem, specifically in the
pons. It is situated in the floor of the fourth ventricle, just under the
cerebellum. This tiny structure serves as the brain's primary source of
norepinephrine, a neurotransmitter crucial for functions such as attention,
arousal, sleep-wake cycles, and memory.
Engborg et al (2025) found "Stress reactivity is modulated by cannabinoid type-1
receptors in norepinephrine and epinephrine neurons in a context-dependent
manner":
"Here, we identify a role for CB1R in NE/E neurons in regulating stress-related
affective responses using a combination of intersectional genetic, anatomical,
behavioral, and physiological approaches. In control mice, Cnr1 mRNA was widely
expressed in medullary C1/A1 and C2/A2 nuclei, with more limited expression in
LC neurons, highlighting molecular diversity within the central noradrenergic
system. Notably, Cnr1 was present in both NE- and E-producing medullary neurons,
marking the first cell-type-specific characterization of Cnr1 in brainstem NE/E
populations and extending prior work focused primarily on the LC (Luskin et al.,
2024, Oropeza et al., 2007, Srivastava et al., 2022, Wyrofsky et al., 2017). In
Cnr1cKO-Dbh mice, Cnr1 expression was reduced across all examined NE/E nuclei.
Behaviorally, Cnr1cKO-Dbh mice exhibited increased center time following
restraint stress, reduced immobility in the forced swim test, heightened active
escape responses to a looming visual threat, and diminished rearing and
ambulation during the initial threat presentation. In contrast, no genotype
differences were observed in the elevated zero maze or light–dark box following
foot shock stress, nor in the tail suspension test. Additionally, heart rate
dynamics remained unchanged. These findings suggest that CB1R signaling in NE/E
neurons modulates behavioral responses to acute stress in a context-dependent
manner."
https://www.sciencedirect.com/science/article/pii/S0306452225008942 [5367]
In "Childhood Trauma is Associated with Poorer
Cognitive Performance in Older Adults" (2018) Petkus et al say:
"Neurobiological mechanisms involving chronic
inflammation, decreased neuroplasticity, and epigenetic modification of
stress-related pathways may explain the possible association between early life
trauma and poorer cognitive performance in later life. The
hypothalamus-pituitary-adrenal (HPA) axis is thought to play a particularly
important role in this association. The HPA axis activates under stress,
resulting in elevated levels of the cortisol hormone and certain severe and/or
chronic stressors, particularly if experienced early in life, may permanently
alter HPA axis function. Studying this association is important, as chronically
elevated cortisol levels have been associated with worse neuropsychological
performance in later life."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6959209/ [3583]
"Perceived stress can have long-term physiological and
psychological consequences
and has shown to be a modifiable risk factor for
Alzheimer disease and related dementias." say Kulshreshtha et al (2023), who
compared perceived stress and health indicators:
"The final analytical sample included 24 448
participants (14 646 women [59.9%]; median age, 64 years [range, 45-98 years];
10 177 Black participants [41.6%] and 14 271 White participants [58.4%]). A
total of 5589 participants (22.9%) reported elevated levels of stress. Elevated
levels of perceived stress (dichotomized as low stress vs elevated stress) were
associated with 1.37 times higher odds of poor cognition after adjustment for
sociodemographic variables, cardiovascular risk factors, and depression
(adjusted odds ratio [AOR], 1.37; 95% CI, 1.22-1.53). The association of the
change in the Perceived Stress Scale score with incident cognitive impairment
was significant in both the unadjusted model (OR, 1.62; 95% CI, 1.46-1.80) and
after adjustment for sociodemographic variables, cardiovascular risk factors,
and depression (AOR, 1.39; 95% CI, 1.22-1.58). There was no interaction with
age, race, and sex."
https://doi.org/10.1001/jamanetworkopen.2023.1860 [3584]
The state of knowledge on species differences shows
that humanity is at an early stage in the understanding of these processes.
https://www.pnas.org/content/pnas/early/2019/12/17/1902288116.full.pdf [149]
But according to Ney et al at the School of
Psychology, University of Tasmania, much of the research as it relates to PTSD
and cannabinoids may be gender-skewed:
"Despite men reportedly experiencing more traumatic
events than women, lifetime prevalence of PTSD is twice as common in women in
Australia (Silove et al., 2017), United Kingdom (Wittchen et al., 2011) and the
United States (Kessler et al., 1995; Tolin Foa, 2006). Whilst exposure to
different trauma types (and specifically interpersonal and sexual violence in
women) makes a substantial contribution, this is insufficient to explain the
difference in prevalence between the sexes (Olff, Langeland, Draijer, & Gersons,
2007; Tolin & Foa, 2006). Despite sex hormones being effectors of stress
responses critical to PTSD aetiology, the majority of psychological and
pharmacological PTSD preclinical research is conducted using males (Lebron-Milad
& Milad, 2012). It is therefore possible that treatments developed for PTSD may
be insensitive to the specific needs of female patients"
See their Table 3 for an overview of studies on sex
differences and endocannabinoid signalling,
https://www.researchgate.net/profile/Luke-Ney-2/publication/326337009_Modulation_of_the_endocannabinoid_system_by_sex_hormones_Implications_for_Posttraumatic_Stress_Disorder/links/5fbd8bfda6fdcc6cc663e25d/Modulation-of-the-endocannabinoid-system-by-sex-hormones-Implications-for-Posttraumatic-Stress-Disorder.pdf
[4387]
Maldonado et al in "The endocannabinoid system in
modulating fear, anxiety, and stress" (2020) explain more about stress and the
ECS:
"Stress is an alteration of homeostasis as a
consequence of external or internal threats. Indeed, acute stressors elicit
immediate and protracted neuroendocrine responses with protective effects. These
responses involve the activation of the sympathetic nervous system and the HPA
axis. Within seconds of stress exposure, noradrenaline and adrenaline are
released through sympathetic postganglionic neurons and adrenal gland chromaffin
cells contributing to fight-or-escape protective responses. In parallel, the HPA
axis is activated through CRH release from the hypothalamus, which leads to ACTH
release from the pituitary gland. ACTH in the general blood stream reaches
adrenal glands that pour glucocorticoids into the blood circulatory system.
These corticoids activate glucocorticoid receptors that increase glucose
availability and trigger transcriptional changes partly directed to limit
inflammation and repair processes that can be postponed.
"The endocannabinoid system present in the HPA axis
and the sympathetic nervous system plays a crucial role in regulating stress
responses (Figure 3). Early studies showed that repeated THC modified dopamine
b-hydroxylase activity in rodent serum, a measure of sympathetic system
activation. This effect was different depending on the basal status of exposed
subjects revealing a complex modulatory role of the endocannabinoid system: THC
alleviated sympathetic activation in naive mice but potentiated this response in
rodents subjected to immobilization stress. CB1R controls peripheral and central
adrenaline, and noradrenaline release involved in stress-induced memory
impairment, and the sympathetic nervous system partly mediates the anxiety-like
effects observed after CB1R blockade. In regard to the HPA axis, pharmacological
and knockout studies demonstrate that CB1R activity limits hypothalamic CRH
release. CB1R is also present in the pituitary gland and adrenal cortex cells,
where it restricts ACTH and glucocorticoid release, respectively. On the
contrary, glucocorticoids induce fast increases in endocannabinoid synthesis in
brain areas that shape the perception of psychological stressors. These regions
include areas involved in cognitive processes such as PFC and hippocampus, and
areas related with affective responses such as the amygdala. Glucocorticoids
released after acute stressors activate G-protein membrane receptors in the BLA,
promoting a rapid increase in retrograde 2-AG signaling that leads to
suppression of GABAergic synaptic inputs onto BLA principal neurons, inducing
fast increases in anxiety-like behavior. These limbic areas are further
connected with the hypothalamus to modulate stress responses (Figure 3). CB1R
located in these structures represent a unique opportunity for pharmacological
modulation. However, the use of exogenous CB1R ligands has been associated with
serious health problems, from THC effects promoting addictive behaviors and
anxiety disorders to the psychiatric alterations (anxiety, depression, or
suicidal behaviors) related to the CB1R inverse agonist rimonabant. Therefore, a
great deal of research has focused on the pharmacological modulation of
endogenous cannabinoids as an alternative approach for the treatment of
stress-induced alterations. In this context, the enzymes involved in the
synthesis and degradation of endocannabinoids represent potential effective
targets with possible better safety profiles than drugs directly acting on
CB1R."
And
"Local CB1R activity has also been associated with
anxiogenesis in certain circuits. Thus, the amygdala sends CB1R -positive
projections to the bed nucleus of the stria terminalis (BNST), a brain region
closely involved in anxiety. This area is connected with midbrain structures,
including the ventral tegmental area and the locus coeruleus. Glutamatergic and
GABAergic projections from the amygdala to BNST are each sufficient for the
development of anxious responses to unpredictable stimuli. CB1R activity in
these projections seems essential for the shift from phasic to sustained fear
responses in fear conditioning chambers, interpreted as a reminiscence of the
human anxiety against unpredictable threats. In the context of an established
anxiogenic response, blocking cannabinoid activity in the BNST facilitates the
transition from persistent to phasic freezing responses, a switch that could
allow earlier reinstatement of normal anxious behavior."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7605023/ [2942]
New data keeps pouring in on THC and it all tends to
support the notion that THC is a fear-reducing substance. More precisely, one
which inhibits the system by which learned fear is retained. Reporting the
"Influence of Δ9-tetrahydrocannabinol on long-term neural correlates of threat
extinction memory retention in humans" (2019) Hammoud et al say:
"...our results are the first to examine the long-term
impact of a single dose administration of THC on the functional activation of
the threat extinction network. Our findings show a significant effect on the
functional connectivity of threat-detection network that emerged after a week
from engagement. These data highlight the need to further investigate the
long-term influence of THC on threat and anxiety circuitry. Specifically, THC,
or compounds with comparable impact on CB1 receptors (e.g., cannabidiol) could
be used as adjuncts to extinction-based therapies for PTSD and anxiety
disorders. This is especially relevant to PTSD treatment given that threat
extinction learning and extinction memory retention has been shown to be
deficient in PTSD patients. Moreover, the neural correlates related to PTSD
psychopathology are comparable to those engaged by THC in the present study."
https://www.nature.com/articles/s41386-019-0416-6.pdf [150]
Among a series of studies of fear extinction involving
Irit Akirev [3987], is "Neuropeptide Y and cannabinoids interaction in the
amygdala after exposure to shock and reminders model of PTSD" from Mayman et al
(2020):
"Modulation of cannabinoid and neuropeptide Y (NPY)
receptors may offer therapeutic benefits for post-traumatic stress disorder
(PTSD). In this study, we aimed to investigate the functional interaction
between these systems in the basolateral amygdala (BLA) in a rat model of PTSD.
"Rats were exposed to the shock and reminders model of
PTSD and tested for hyper arousal/PTSD- and depression-like behaviors 3 weeks
later. Immediately after shock exposure rats were microinjected into the BLA
with URB597, a selective inhibitor of fatty acid amide hydrolase (FAAH) that
increases the levels of the endocannabinoid anandamide or with the NPY1 receptor
agonist Leu31,Pro34-NPY (Leu).
"Intra-BLA URB597 prevented the
shock/reminders-induced PTSD- behaviors (extinction, startle) and
depression-behaviors (despair, social impairments). These preventing effects of
URB597 on PTSD- and depression-like behaviors were shown to be mostly mediated
by cannabinoid CB1 and NPY1 receptors, as they were blocked when URB597 was
co-administered with a low dose of a CB1 or NPY1 receptor antagonist. Similarly,
intra-BLA Leu prevented development of all the behaviors. Interestingly, a CB1
antagonist prevented the effects of Leu on despair and social behavior, but not
the effects on extinction and startle. Moreover, exposure to shock and reminders
upregulated CB1 and NPY1 receptors in the BLA and infralimbic prefrontal cortex
and this upregulation was restored to normal with intra-BLA URB597 or Leu.
"The findings suggest that the functional interaction
between the eCB and NPY1 systems is complex and provide a rationale for
exploring novel therapeutic strategies that target the cannabinoid and NPY
systems for stress-related diseases."
https://www.sciencedirect.com/science/article/abs/pii/S0028390819303661
[3989]
In 2025, 100 years since General Smuts got his way at the Opium Convention, Xue
et al were happy to reveal "An Amygdala-hippocampus Circuit for Endocannabinoid
Modulation of Anxiety Avoidance":
"Recent studies indicate a therapeutic potential of increased brain
endocannabinoids (eCBs) in anxiety disorders, but the underlying brain circuits
are still elusive. Here, it is observed that optogenetic inhibition and
activation of anterior basolateral amygdala (aBLA) - ventral hippocampus (vHPC)
glutamatergic projections respectively decrease and increase anxiety avoidance
behaviors. Then, the contributions of eCBs in aBLA–vHPC projections to anxiety
avoidance are investigated by employing three newly developed synapse- and
circuit-specific eCB-targeted viral strategies to achieve real-time monitoring
of eCB release, in vivo optogenetic activation of CB1 receptors, and CRISPR-Cas9
gene knockdown of eCB biosynthesis enzymes. Prominent eCB release are
surprisingly found at aBLA–vHPC glutamatergic synapses during anxiety avoidance,
suggesting inhibitory effects of increased eCBs in aBLA–vHPC projections on
anxiety avoidance. This idea is further supported by findings that specific
activation of CB1 receptors at aBLA–vHPC synapses inhibit presynaptic glutamate
release and reduce anxiety avoidance. In contrast, specific knockdown of eCB
biosynthesis enzymes at aBLA–vHPC synapses reduce eCB levels at aBLA–vHPC
glutamatergic synapses and increase anxiety avoidance. Additionally, inhibition
of aBLA-innervated vHPC glutamatergic neurons alleviates anxiety avoidance.
Together, these findings reveal counteracting effects of increased eCB signaling
in aBLA–vHPC circuits on anxiety avoidance."
https://advanced.onlinelibrary.wiley.com/doi/pdfdirect/10.1002/advs.202505121
[5521]
Nobuo Masataka (2025) frightened some naive cats with fake thunderstorms. CBD
helped:
"In humans, cannabidiol (CBD), the primary non-addictive component of cannabis,
is known to possess considerable therapeutic potential. The purpose of this
study was to investigate the effects of CBD administration on reducing
sound-induced fear in healthy domestic cats in a laboratory model of
thunderstorm simulation. A total of 40 cats, each naďve to the current testing,
were randomly assigned into either of two administration groups (CBD and
placebo). Each group was then exposed to the thunderstorm test twice; once at
the beginning of the administration (the administration of CBD at 4.0 mg/kg/day
over a 2-week-period or the administration of the same amount of sunflower oil
as a placebo) and once after the end of the administration. When undesirable
urination was observed, occurrences of this behaviour were found to decrease
significantly when CBD was administered. However, no such changes were recorded
when the placebo was administered. These results indicate that CBD could be an
effective option for the treatment of noise-induced fear."
https://www.mdpi.com/2076-2615/15/11/1642 [5341]
For "Cannabidiol Treatment in a Predator-Based Animal
Model of PTSD: Assessing Oxidative Stress and Memory Performance" Jîtcă et al
(2025) found:
"CBD exhibited a tendency to reduce anxiety, a common
symptom of PTSD, although this effect was not statistically significant.
However, it demonstrated protective effects on memory, as evidenced by the MWM
test. Likewise, CBD also showed a reduction in MDA levels, which implies that an
improvement in PTSD symptomatology may also target a reduction in oxidative
stress. Since there are several models used to induce PTSD, we cannot consider
that one is better than the other, because each brings an advantage, which
allows us to create a picture of the mechanisms involved in the occurrence of
PTSD and how the symptoms can be improved. An important direction of this topic
could be the investigation of the molecular mechanisms by which CBD influences
PTSD symptoms, including the analysis of the expression of genes and proteins
involved in the stress response, neuroinflammation and neuroplasticity (BDNF)
and inflammatory markers (IL-6, TNF-α) in order to provide additional
information about the mode of action of CBD."
https://www.mdpi.com/1422-0067/26/10/4491/pdf?version=1746705743 [5034]
Then there was Sultan et al (2025) "Controlled Inhalation of
Tetrahydrocannabinol-Predominant Cannabis Flos Mitigates Severity of
Post-Traumatic Stress Disorder Symptoms and Improves Quality of Sleep and
General Mood in Cannabis-Experienced UK Civilians: A Real-World, Observational
Study". Beginning with the observation that "Approximately 4% of the UK
population experiences PTSD", this study of 58 victims is outlined in Figure 1,
showing improvements in global PTSD score, intrusion, avoidance, cognition and
mood, and hyperreactivity/hyperarousal:
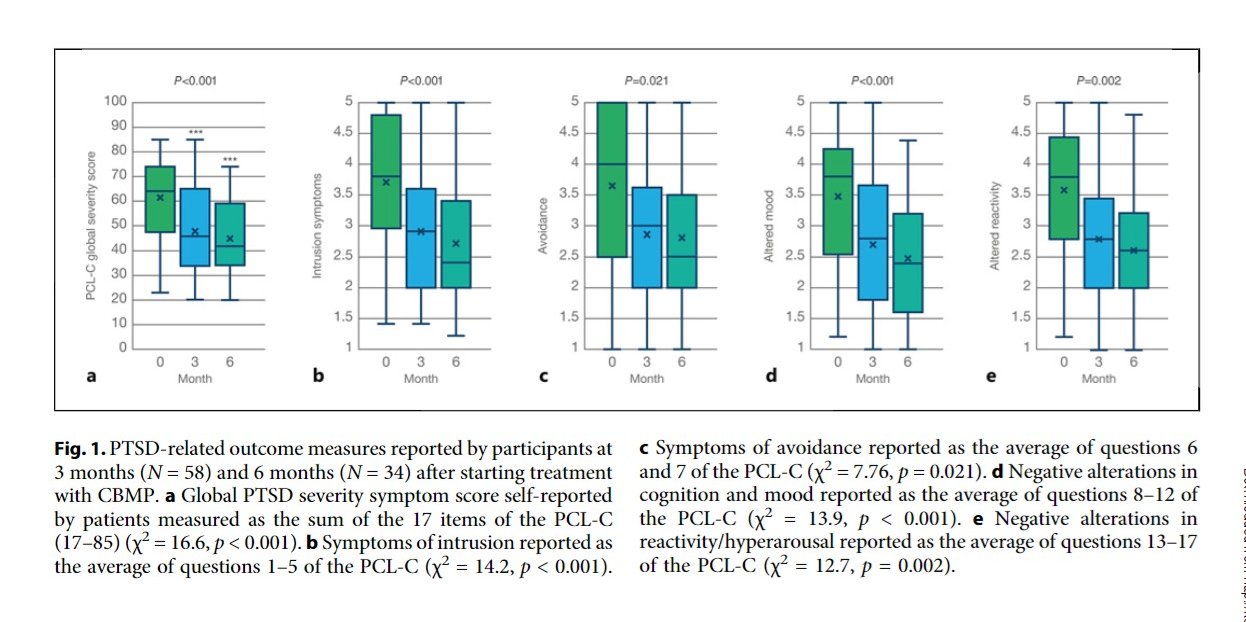
https://karger.com/mca/article-pdf/7/1/149/4282163/000540978.pdf [5106]
"Endocannabinoids inhibit contextual fear memory generalization via hippocampal
GABAergic synaptic transmission" report Ge et al (2025):
"Memory generalization allows an organism to adapt to new conditions, but
overgeneralization of fear or traumatic experiences can be detrimental to
survival and contributes to the development of various mental disorders.
However, the cellular and molecular mechanisms underlying fear memory
generalization, especially in the hippocampus, remain largely unknown. In this
study, utilizing a well-established mouse model of fear memory generalization,
we investigated the role of endocannabinoids (eCBs)-mediated GABAergic synaptic
inputs to hippocampal pyramidal neurons in regulating contextual fear memory
generalization. Our results revealed that pharmacological or genetic blockade of
CB1R in hippocampal CA1 resulted in overgeneralization of contextual fear memory
but not fear memory expression. Subsequent investigations in conditional
knockout mice revealed the involvement of CB1R in GABAergic neurons, but not
those in glutamatergic neurons or astrocytes, in this overgeneralization. In
addition, activation of GABAA receptors on pyramidal neurons was required for
inducing overgeneralization via AM281, a CB1R antagonist. Neural mechanistic
studies showed that eCBs/CB1R signaling regulates both the activity and
plasticity of inhibitory synapses during generalization, highlighting the
prominence of the disinhibition of CB1R in interneurons during this process.
Subsequently, we delved into the downstream effects and found that eCB-dependent
long-term potentiation (LTP) in CA1 pyramidal neurons was regulated by the
aforementioned mechanisms. Our findings illustrate that the eCBs/CB1R signaling
pathway modulates the balance between fear memory discrimination and
generalization by controlling inhibitory inputs to hippocampal pyramidal
neurons, accompanied by alterations in excitatory plasticity within this
region."
https://www.pnas.org/doi/10.1073/pnas.2423974122 [5254]
"Medical Cannabis Improved PTSD Symptoms, Anxiety, and Quality of Life Over an
18-Month Period" say Datta et al (2025):
"In 269 patients, significant improvements in PTSD symptoms, anxiety, sleep
quality, and HRQoL were observed at all follow-up points (p < 0.001). On
multivariate logistic regression, male gender (OR = 0.51; 95% CI:0.28–0.94;
p = 0.034) was associated with a reduced chance of reporting improvements in
IES-R. Adverse events were reported by 70 (26.02%) patients, with insomnia
(n = 42, 15.61%) and fatigue (n = 40, 14.87%) being the most common."
Nevertheless sleep quality scale (SQS) improved significantly, along with nearly
all other parameters: avoidance, intrusions, hyperarousal, self-care, usual
activities, pain and discomfort, anxiety and depression, generalized anxiety
disorder‐7 (GAD-7), patient global impression of change (PGIC) and impact of
event scale – revised (IES-R) total score at all follow-up points: 1, 3, 6, 12
and 18 months.
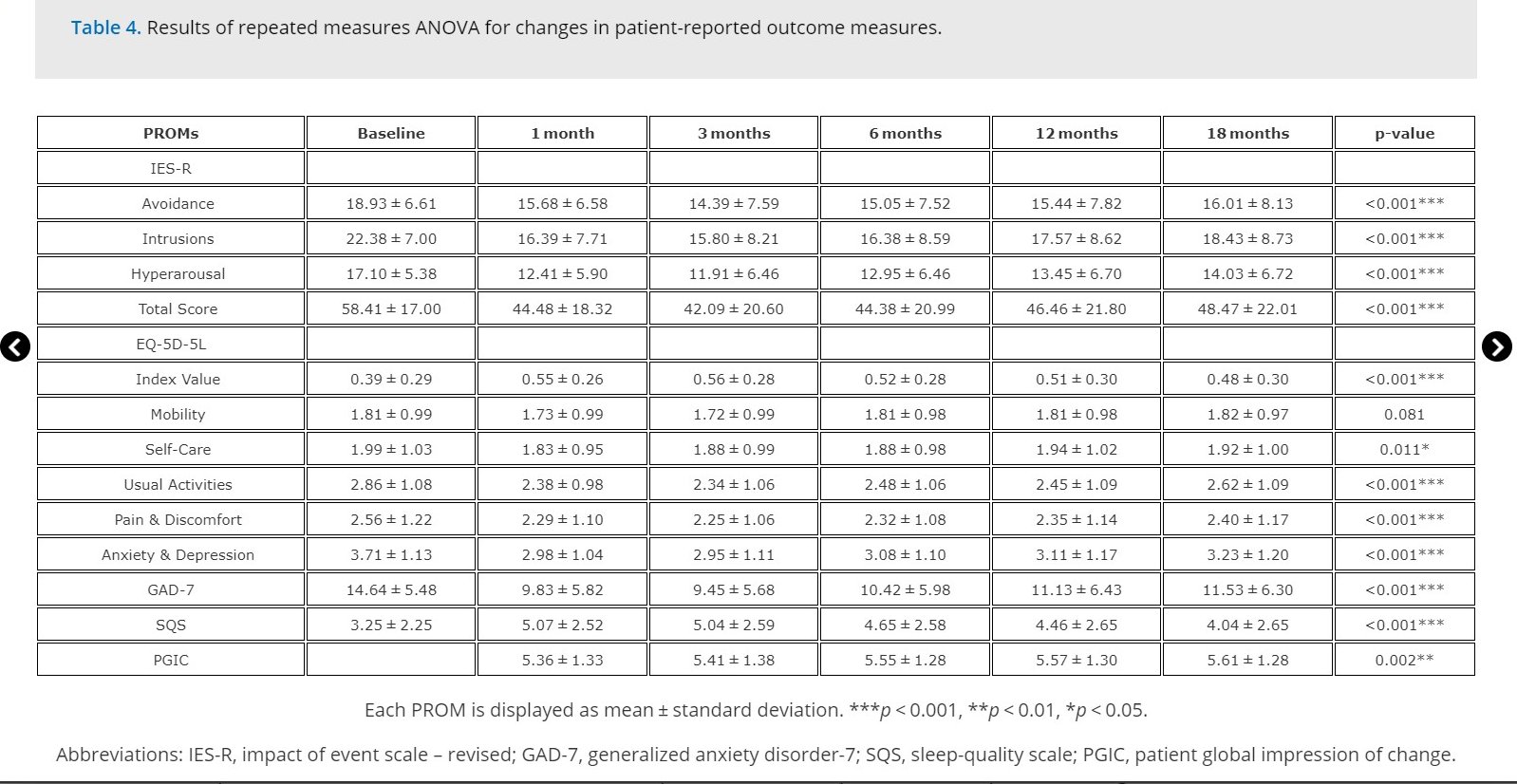
https://www.tandfonline.com/doi/full/10.1080/14737175.2025.2490539#d1e649
[5179]
Diurnal variations in endocannabinoids
https://pubmed.ncbi.nlm.nih.gov/31610409/ [53]
Shows daily variation in endocannabinoids, the effect
of circadian rhythms, on AEA, 2-AG and congeners OEA and PEA.
"Congeners of AEA, the structural analogs
oleoylethanolamide (OEA) and palmitoylethanolamide (PEA) were simultaneously
assayed. Prior to 24-h blood sampling, each participant was exposed to two
nights of normal (8.5 h) or restricted sleep (4.5 h). The two sleep conditions
were separated by at least one month. In both sleep conditions, during the
period of blood sampling, each individual ate the same high-carbohydrate meal at
0900, 1400, and 1900.
"Results: Mean 24-h concentrations of AEA were 0.697 ±
0.11 pmol/ml. A reproducible biphasic 24-h profile of AEA was observed with a
first peak occurring during early sleep (0200) and a second peak in the
mid-afternoon (1500) while a nadir was detected in the mid-morning (1000). The
24-h profiles for both OEA and PEA followed a similar pattern to that observed
for AEA. AEA, OEA, and PEA levels were not affected by sleep restriction at any
time of day, contrasting with the elevation of early afternoon levels previously
observed for 2-AG.
"Conclusions: The 24-h rhythm of AEA is markedly
different from that of 2-AG, being of lesser amplitude and biphasic, rather than
monophasic. These observations suggest distinct regulatory pathways of the two
eCB and indicate that time of day needs to be carefully controlled in studies
attempting to delineate their relative roles. Moreover, unlike 2-AG, AEA is not
altered by sleep restriction, suggesting that physiological perturbations may
affect AEA and 2-AG differently. Similar 24-h profiles were observed for OEA and
PEA following normal and restricted sleep, further corroborating the validity of
the wave-shape and lack of response to sleep loss observed for the AEA profile.
Therapeutic approaches involving agonism or antagonism of peripheral eCB
signaling will likely need to be tailored according to time of day."
These two papers tell us that a) reduced EC is a
reliable marker of PTSD; b) more AEA correlates with less symptoms of PTSD; c)
AEA behaves differently in its diurnal behaviour; and d) any perceived need for
exogenous supplementation of EC is likely to be time of day dependent.
"In a study of the effects of THC on fear extinction,
Compared to subjects who received placebo, participants who received THC showed
increased vmPFC and HIPP activation to a previously extinguished conditioned
stimulus (CS+E) during extinction memory recall."
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC3960373&blobtype=pdf
[146]
Another study using MRI and a well-established
threat-processing paradigm found that low doses of ∆9-tetrahydrocannabinol (THC)
can produce anxiolytic effects, reduce threat-related amygdala activation, and
enhance functional coupling between the amygdala and medial prefrontal cortex
and adjacent rostral cingulate cortex (mPFC/rACC) during threat processing in
healthy adults.
https://pubmed.ncbi.nlm.nih.gov/32162103/ [147]
Recognising the cannabis (but not its illegality)
sometimes produces anxiety, in 2015 Komaki et al of the Neurophysiology Research
Center, Hamadan University of Medical Sciences, Iran, evaluated anxiety and CB1
effects:
"Previous studies have shown that [the]
cannabinoidergic system is involved in anxiety. However, there are controversial
reports in the experimental studies. The aim of this study is to evaluate the
effect of pharmacological stimulation or blocking of CB1 receptors and
inhibition of endocannabinoid degradation in anxiety like behavior in elevated
plus-maze (EPM) test in rat. The EPM is one of the most widely used animal
models of anxiety.
"Male Wistar rats were randomly allocated to ten
groups. Different groups of animals intraperitoneally received Win-55212 (0.3, 1
and 5 mg/kg) as CB1 receptor agonist, AM-251 (0.3, 1 and 5 mg/kg) as CB1
receptor antagonist, URB-597 (0.03, 0.1 and 0.3 mg/kg) as endocannabinoid
breakdown inhibitor or saline (as control group) 30 min before submitting into
EPM test.
"The results showed that compared to the control
group, Win-55212 (1 and 5 mg/kg) and URB-597 (0.1 and 0.3 mg/kg) significantly
increased both of the time and percentage of entries into open arms. AM-251 (1
and 5 mg/kg) significantly decreased the time and percentage of entries into
open arms in the EPM test. These substances have no effects on the total
distance covered by animals and number of closed arm entries.
"It is concluded that activation of cannabinoid
receptor exert anxiolytic effect while blocking of cannabinoid receptor resulted
in anxiety behavior. The locomotor activity was not significantly changed by
cannabinoid system. It is suggested that potentiation of cannabinoid system may
be therapeutic strategy for the anxiety behavior."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4656987/ [2108]
In 2010 El-Alfy et al at the University of Mississippi
had tried some different anxiety tests:
"The antidepressant action of cannabis as well as the
interaction between antidepressants and the endocannabinoid system has been
reported. This study was conducted to assess the antidepressant-like activity of
Δ9-THC and other cannabinoids. Cannabinoids were initially evaluated in the
mouse tetrad assay to determine doses that do not induce hypothermia or
catalepsy [a neurological finding of prolonged muscular rigidity and immobility
with decreased response to external stimuli and reduced sensitivity to pain].
The automated mouse forced swim (FST) and tail suspension (TST) tests were used
to determine antidepressant action. At doses lacking hypothermic and cataleptic
effects (1.25, 2.5, and 5 mg/kg, i.p.), both Δ9-THC and Δ8-THC showed a U-shaped
dose response with only Δ9-THC showing significant antidepressant-like effects
at 2.5 mg/kg (p < 0.05) in the FST. The cannabinoids cannabigerol (CBG) and
cannabinol (CBN) did not produce antidepressant-like actions up to 80 mg/kg in
the mouse FST, while cannabichromene (CBC) and cannabidiol (CBD) exhibited
significant effect at 20 and 200 mg/kg, respectively (p < 0.01). The
antidepressant-like action of Δ9-THC and CBC was further confirmed in the TST.
Δ9 -THC exhibited the same U-shaped dose response with significant
antidepressant-like action at 2.5 mg/kg (p < 0.05) while CBC resulted in a
significant dose dependent decrease in immobility at 40 and 80 mg/kg doses (p <
0.01). Results of this study show that Δ9-THC and other cannabinoids exert
antidepressant-like actions, and thus may contribute to the overall
mood-elevating properties of cannabis."
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC2866040&blobtype=pdf
[2109]
Akirav (2013) summarised the resilience-promoting
properties of cannabinoids thus:
"Glucocorticoid and endocannabinoid systems cross-talk
after stress.
Exogenous cannabinoid agonists decrease HPA axis
activity after stress.
Stress and glucocorticoids modulate endocannabinoid
levels in limbic areas.
Cannabinoid receptor agonists ameliorate the effects
of stress on emotional memory.
Cannabinoids decrease HPA axis activity in the
amygdala via the GABAergic system."
She proposed the involvement of the amygdala:
"Enhancing cannabinoids signaling using exogenous CB1
receptor agonists prevent the effects of acute stress on emotional memory. I
propose a model suggesting that the ameliorating effects of exogenously
administered cannabinoids on emotional learning after acute stress are mediated
by the decrease in the activity of the HPA axis via GABAergic mechanisms in the
amygdala."
... which we shall see was later confirmed below.
https://www.sciencedirect.com/science/article/abs/pii/S0149763413001929?via%3Dihub
[3986]
On "Neuroplasticity in Posttraumatic Stress Disorder"
López-López and Crespo (2025) (machine translated from Spanish) tell us:
"Resilience, understood as the dynamic adaptation
following trauma, is a determining factor in the vulnerability to develop PTSD
that may be associated with myelination. It has been described that contextual
fear memory, like other memories, requires the generation of new myelin;
therefore, the use of promyelinating drugs such as clemastine fumarate in mice
improves remote memory recall and favors fear generalization. In war veterans
with and without PTSD, estimating the degree of myelination through
T1/T2-weighted magnetic resonance imaging, a positive correlation has been
observed between the total index of the Clinician-Administered PTSD Scale (CAPS)
and myelination in the hippocampus. Furthermore, this same correlation is
observed regarding the severity of depressive symptoms.
"A recent translational study focusing on the
hippocampus, amygdala and corpus callosum described similar results in rats and
humans. In rodents, analysis of myelination in the gray matter of the
hippocampal dentate gyrus shows a positive correlation between oligodendrocyte
density and myelin basic protein, a protein that is translated only in mature
myelinating oligodendrocytes, and the avoidance and anxiety phenotype, while in
the amygdala and cornu ammonis (CA) regions of the hippocampus this positive
correlation occurs with contextual fear learning. This corroborates data from a
previous study using this same protein, together with specific oligodendrocytes
of the hippocampal dentate gyrus, showing that they are associated with
hypervigilance, avoidance and escape in the face of stress from two weeks after
its onset."
https://pmc-ncbi-nlm-nih-gov.translate.goog/articles/PMC12326437/?_x_tr_sl=auto&_x_tr_tl=en&_x_tr_hl=sl
[5246]
Zhu et al (2025) add that:
"The bed nucleus of stria terminalis (BNST) acts as a
crucial hub for assessing vigilant threats, with the oval subnucleus (ovBNST)
being enriched in endocannabinoid ligands and receptors. The endocannabinoid
system (ECS) is well recognized for its role in stress responses. However, the
molecular and circuitry mechanisms through which the ovBNST ECS mediates chronic
stress induced depressive phenotypes remain unclear.
"Methods and results: The chronic unpredictable mild
stress (CUMS) was optimized to model the depression-like behaviors and body
weight loss in mice. By utilizing the endocannabinoid sensor, an increased
release of endocannabinoid in the ovBNST was probed in response to acute stress.
Local blockage of ovBNST cannabinoid type 1 receptor (CB1R) with NESS0327
induced both anhedonia and despair depressive phenotypes in naďve mice. In
contrast, intra-ovBNST infusion of either CB1R agonist or cannabinoid hydrolase
inhibitor JZL-184 ameliorated despair-like behaviors while merely changed
anhedonia in CUMS mice. By combining viral tracing with RNAscope and western
blotting, the reduction in CB1R transcriptional and translational level was
found to be associated with the CUMS induced depressive disorders. This
reduction may be attributed to the changes in ovBNST located presynaptic CB1R
that originates from the medial prefrontal cortex (mPFC).
"Discussion: Overall, these results suggest that
chronic stress may restructure the ovBNST ECS to result in depressive
phenotypes. This study may extend the comprehension of ECS in the ovBNST,
specifically its role in modulating the pathogenesis of depressive disorders
induced by chronic stress."
https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1629351/full
[5271]
According to Forsythe and Boileau in "Use of
cannabinoids for the treatment of patients with post-traumatic stress disorder"
(2021):
"Numerous treatment options have been developed for
the disorder, including psychotherapeutic approaches such as exposure therapy,
virtual reality therapy, cognitive behavioral therapies and eye movement
desensitization and reprocessing. Around 40–70% of individuals receiving these
treatments briefly have noticed significant improvement in symptoms and
extinction of the learned fear. Not all individuals are ideal candidates for
these treatments, however. High rates of suicidality, dissociation, destructive
impulsivity, and chaotic life problems are indications that the patients may not
respond well to treatment, causing clinicians to become more likely to forgo
attempting these therapies. This exposes a need for developing other therapy
options."
https://www.degruyter.com/document/doi/10.1515/jbcpp-2020-0279/html [3546]
"SSRIs have long been considered first-line
pharmacological treatment for PTSD; however, only about 60% of patients respond
to it with only 20–30% reaching full remission. The most promising agents to aid
in the process of improving PTSD symptoms were found to target receptors such as
the N-methyl-D-aspartic acid (NMDA) receptor, the receptors targeted by
3,4-methylenedioxyN-methylamphetamine (MDMA), such as the 5HT2 receptor, and the
endocannabinoid CB1 receptor."
Ten studies THC, CBD or synthetic cannabinoids are
summarised in Table 1.
"A common, and expected, limitation of these studies
is small sample size."
https://www.degruyter.com/document/doi/10.1515/jbcpp-2020-0279/pdf [297]
As Rabinak et al (2020) reported in "Cannabinoid
modulation of corticolimbic activation to threat in trauma-exposed adults: a
preliminary study":
"In adults with PTSD, THC lowered threat-related
amygdala reactivity, increased mPFC activation during threat, and increased
mPFC-amygdala functional coupling." said Wayne State University Detroit
researchers Rabinak et al in "Cannabinoid modulation of corticolimbic activation
to threat in trauma-exposed adults: a preliminary study" (2020). "During fMRI
scanning, participants completed an emotional face processing task developed by
Hariri and colleagues (Hariri et al. 2002) that has been shown to reliably
elicit threat-related amygdala responses."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7244361/ [4558]
"In adults with PTSD, THC lowered threat-related
amygdala reactivity, increased mPFC activation during threat, and increased
mPFC-amygdala functional coupling." said Wayne State University Detroit
researchers Rabinak et al in "Cannabinoid modulation of corticolimbic activation
to threat in trauma-exposed adults: a preliminary study" (2020). "During fMRI
scanning, participants completed an emotional face processing task developed by
Hariri and colleagues (Hariri et al. 2002) that has been shown to reliably
elicit threat-related amygdala responses."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7244361/ [4558]
In 2019, Lake et al of the British Columbia Centre on
Substance Use asked "Does cannabis use modify the effect of post-traumatic
stress disorder on severe depression and suicidal ideation? Evidence from a
population-based cross-sectional study of Canadians". And the answer was yes.
"Among 24,089 eligible respondents, 420 (1.7%)
reported a current clinical diagnosis of post-traumatic stress disorder. In
total, 106 (28.2%) people with post-traumatic stress disorder reported past-year
cannabis use, compared to 11.2% of those without post-traumatic stress disorder
(p < 0.001). In multivariable analyses, post-traumatic stress disorder was
significantly associated with recent major depressive episode (adjusted odds
ratio = 7.18, 95% confidence interval: 4.32–11.91) and suicidal ideation
(adjusted odds ratio = 4.76, 95% confidence interval: 2.39–9.47) among cannabis
non-users. post-traumatic stress disorder was not associated with either outcome
among cannabis-using respondents (both p > 0.05)."
https://journals.sagepub.com/doi/abs/10.1177/0269881119882806 [4560]
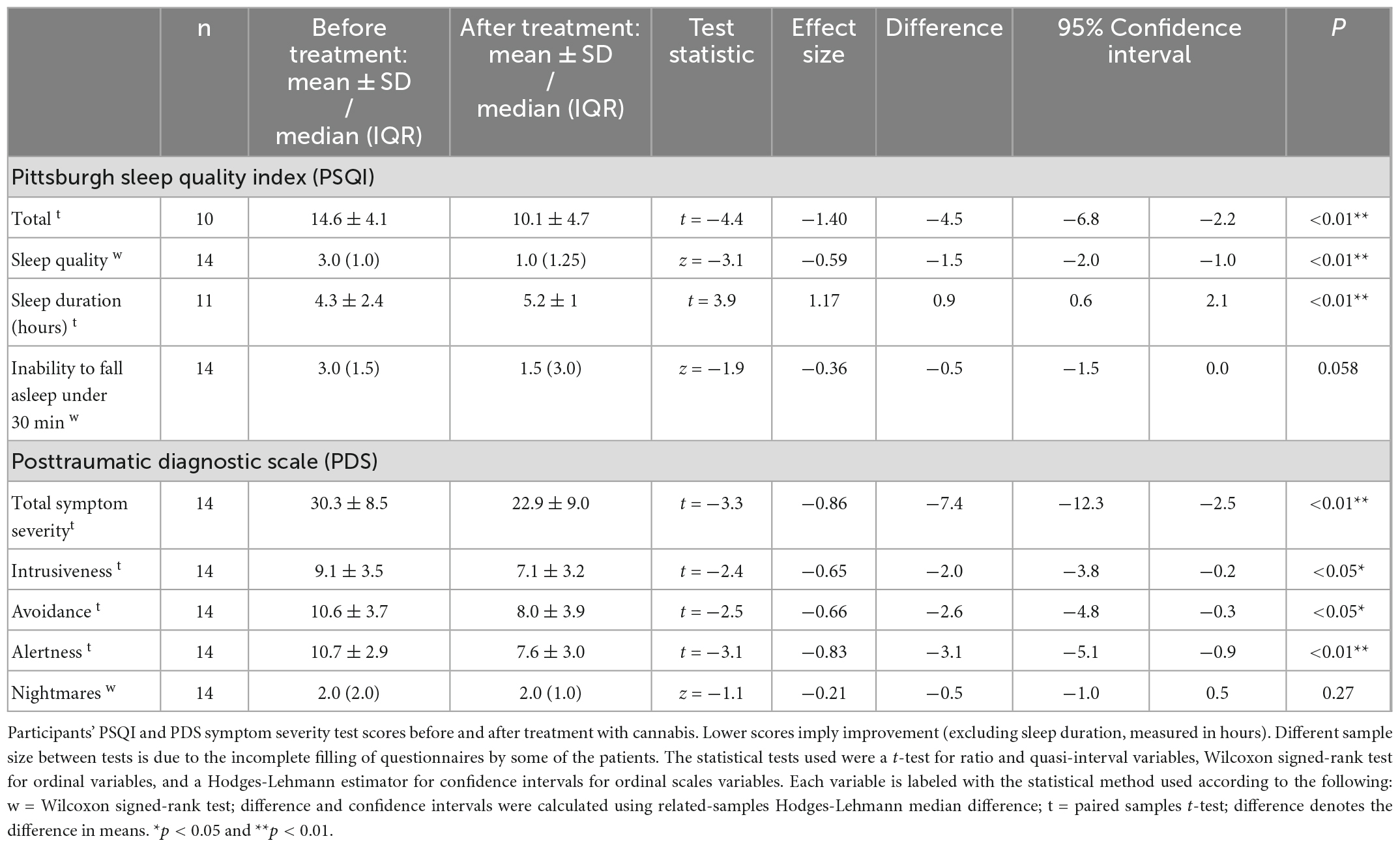
Nacasch et al (2022) targeted the endocannabinoid
system in treatment-resistant combat PTSD:
"In this retrospective naturalistic study, we followed
14 relatively mature (32-68 years of age), treatment-resistant, chronic combat
post-traumatic patients who remained severely symptomatic despite treatment with
many lines of conventional treatment prior to receiving medicinal cannabis. Our
findings show that total sleep score, subjective sleep quality, and sleep
duration significantly improved (p < 0.01). Total PTSD symptom score and its
subdomains (intrusiveness, avoidance, and alertness) showed improvement (p <
0.05). However, there was no improvement in the frequency of nightmares (p =
0.27). The mean follow-up time was 1.1 ± 0.8 years (range of 0.5 to 3 years)."
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2022.1014630/full
[4559]
In "Self-reported Medicinal Cannabis Use as an
Alternative to Prescription and Over-the-counter Medication Use Among US
Military Veterans" (2023) McNabb et al examined a mostly RML-friendly
Massachusetts-based cohort of ex-armed forces personnel, reporting in Clinical
Therapeutics.
"A total of 510 veterans of US military service
participated in the survey, which was administered between March 3 and December
31, 2019. The participants reported experiencing a variety of mental and other
physical health conditions. Primary health conditions reported included chronic
pain (196; 38%), PTSD (131; 26%), anxiety (47; 9%), and depression (26; 5%).
Most participants (343; 67%) reported using cannabis daily. Many reported using
cannabis to reduce the use of over-the-counter medications (151; 30%) including
antidepressants (130; 25%), anti-inflammatories (89; 17%), and other
prescription medications. Additionally, 463 veterans (91% of respondents)
reported that medical cannabis helped them to experience a greater quality of
life and 105 (21%) reported using fewer opioids as a result of their medical
cannabis use. Veterans who were Black, who were female, who served in active
combat, and who were living with chronic pain were more likely to report a
desire to reduce the number of prescription medications they were taking (odds
ratios = 2.92, 2.29, 1.79, and 2.30, respectively). Women and individuals who
used cannabis daily were more likely to report active use of cannabis to reduce
prescription medication use (odds ratios = 3.05 and 2.26)."
https://www.clinicaltherapeutics.com/article/S0149-2918(23)00133-9/fulltext
[2859]
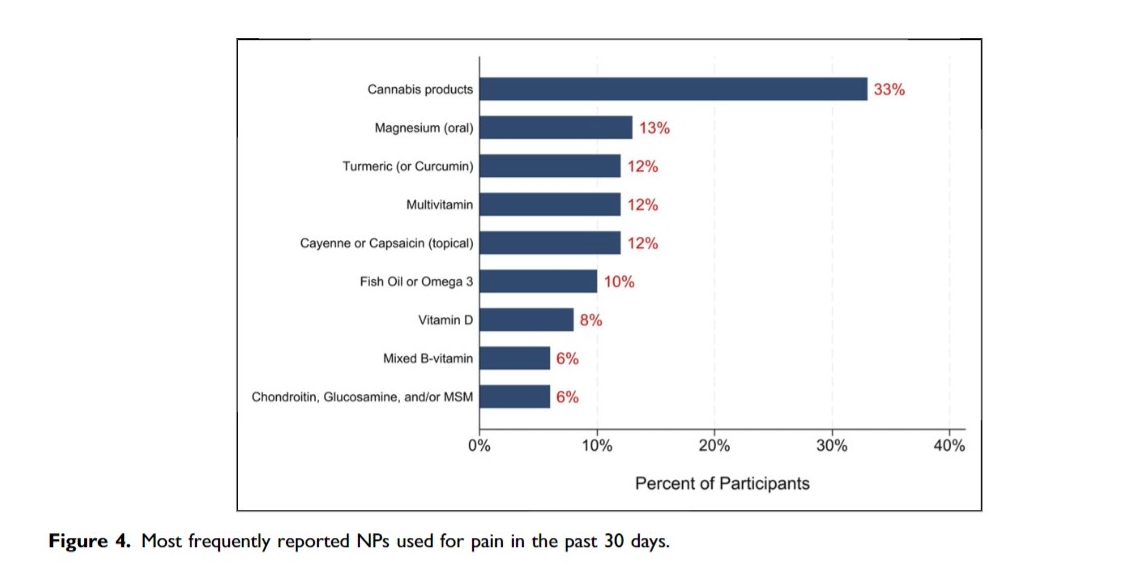
Another survey of 52 veterans, all with chronic pain,
found that cannabis was the most frequently used natural products, followed by
magnesium and turmeric (or curcumin) and vitamins.
https://escholarship.org/content/qt4896q9pd/qt4896q9pd_noSplash_62d21e2a7124ce26aee1df003cbcfb0f.pdf?t=ssqyzq
[4841]
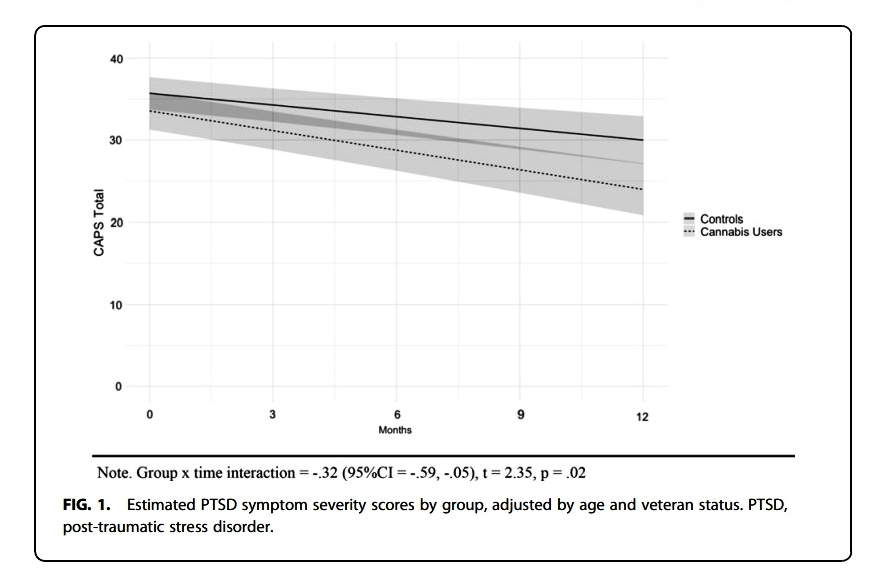
In the USA Bonn-Miller et al (2022)
"...assessed PTSD symptoms and functioning every 3
months over the course of a year in two samples of participants diagnosed with
PTSD: (1) those with PTSD using dispensary-obtained cannabis (cannabis users)
and (2) those with PTSD, who do not use cannabis (controls). Linear
mixed-effects models and generalized estimating equations tested whether
trajectories of symptoms differed between the two subsamples.
"Results: A total of 150 participants (mean [standard
deviation] age, 50.67 [15.26] years; 73% male) were enrolled in the study. Over
the course of 1 year, the cannabis users reported a greater decrease in PTSD
symptom severity over time compared to controls [group×time interaction=−0.32
(95% confidence interval [CI]=−0.59 to −0.05, R2=0.13; t=−2.35, p=0.02).
Participants who used cannabis were 2.57 times more likely to no longer meet
DSM-5 criteria for PTSD at the end of the study observation period compared to
participants who did not use cannabis (95% CI=1.12–6.07; p=0.03)."
and
"Adjusting for age and veteran status, cannabis users
showed a significantly greater rate of decline for hyperarousal symptoms
compared to controls."
https://www.ptsd.va.gov/professional/articles/article-pdf/id1563675.pdf
[2104]
In Israel, Nasach et al examined "Medical cannabis for
treatment-resistant combat PTSD" (2023).
"In this retrospective naturalistic study, we followed
14 relatively mature (32-68 years of age), treatment-resistant, chronic combat
post-traumatic patients who remained severely symptomatic despite treatment with
many lines of conventional treatment prior to receiving medicinal cannabis. Our
findings show that total sleep score, subjective sleep quality, and sleep
duration significantly improved (p < 0.01). Total PTSD symptom score and its
subdomains (intrusiveness, avoidance, and alertness) showed improvement (p <
0.05). However, there was no improvement in the frequency of nightmares (p =
0.27). The mean follow-up time was 1.1 ± 0.8 years (range of 0.5 to 3 years)."
https://www.frontiersin.org/articles/10.3389/fpsyt.2022.1014630 [2359]
McNabb et al examined "Self-reported Medicinal
Cannabis Use as an Alternative to Prescription and Over-the-counter Medication
Use Among US Military Veterans" (2023):
"A total of 510 veterans of US military service
participated in the survey, which was administered between March 3 and December
31, 2019. The participants reported experiencing a variety of mental and other
physical health conditions. Primary health conditions reported included chronic
pain (196; 38%), PTSD (131; 26%), anxiety (47; 9%), and depression (26; 5%).
Most participants (343; 67%) reported using cannabis daily. Many reported using
cannabis to reduce the use of over-the-counter medications (151; 30%) including
antidepressants (130; 25%), anti-inflammatories (89; 17%), and other
prescription medications. Additionally, 463 veterans (91% of respondents)
reported that medical cannabis helped them to experience a greater quality of
life and 105 (21%) reported using fewer opioids as a result of their medical
cannabis use. Veterans who were Black, who were female, who served in active
combat, and who were living with chronic pain were more likely to report a
desire to reduce the number of prescription medications they were taking (odds
ratios = 2.92, 2.29, 1.79, and 2.30, respectively). Women and individuals who
used cannabis daily were more likely to report active use of cannabis to reduce
prescription medication use (odds ratios = 3.05 and 2.26)."
and
In line with previous research and VA statistics, the
participants in this study experienced several mental and other physical health
concerns. Many reported experiences with PTSD, exposure to occupational
environmental hazards (eg, agent orange, asbestos, burn pits), chronic pain,
anxiety, and depression, among other conditions. Study findings also revealed
that participants' cannabis use positively affected the treatment or management
of several health conditions and symptoms. Many of the respondents reported that
medicinal cannabis treatment helped them to experience a greater quality of
life, fewer psychological symptoms, fewer physical symptoms, and to use less
alcohol, fewer medications, less tobacco, and fewer opioids.
https://www.clinicaltherapeutics.com/article/S0149-2918(23)00133-9/fulltext#seccesectitle0001
[2823]
According to Lynskey et al (2024):
"Background
Cannabis-based medicinal products (CBMPs) are
increasingly being used to treat post-traumatic stress disorder (PTSD), despite
limited evidence of their efficacy. PTSD is often comorbid with major
depression, and little is known about whether comorbid depression alters the
effectiveness of CBMPs.
"Aims
To document the prevalence of depression among
individuals seeking CBMPs to treat PTSD and to examine whether the effectiveness
of CBMPs varies by depression status.
"Method
Data were available for 238 people with PTSD seeking
CBMP treatment (5.9% of the treatment-seeking sample) and 3-month follow-up data
were available for 116 of these. Self-reported PTSD symptoms were assessed at
treatment entry and at 3-month follow-up using the PTSD Checklist – Civilian
Version (PCL-C). The probable presence of comorbid depression at treatment entry
was assessed using the nine-item Patient Health Questionnaire (PHQ-9).
Additional data included sociodemographic characteristics and self-reported
quality of life.
"Results
In total, 77% met screening criteria for depression,
which was associated with higher levels of PTSD symptomatology (mean 67.8 v.
48.4, F(1,236) = 118.5, P < 0.001) and poorer general health, quality of life
and sleep. PTSD symptomatology reduced substantially 3 months after commencing
treatment (mean 58.0 v. 47.0, F(1,112) = 14.5, P < 0.001), with a significant
interaction (F(1,112) = 6.2, P < 0.05) indicating greater improvement in those
with depression (mean difference 15.3) than in those without (mean difference
7).
"Conclusions
Depression is common among individuals seeking CBMPs
to treat PTSD and is associated with greater symptom severity and poorer quality
of life. Effectiveness of CBMPs for treating PTSD does not appear to be impaired
in people with comorbid depression."
https://www.cambridge.org/core/journals/bjpsych-open/article/medicinal-cannabis-for-treating-posttraumatic-stress-disorder-and-comorbid-depression-realworld-evidence/F88B15F3E00576E757ADF4915F9874A6
[4483]
In a larger study "Suicidal Ideation in Medicinal
Cannabis Patients: A 12-Month Prospective Study" (2024) the objective of Lynskey
et al was...
"Objective
To document the prevalence and correlates of suicidal
ideation (SI) among individuals seeking cannabis-based medicinal products
(CBMPs); to test whether SI declines or intensifies after three months of CBMP
treatment and to document 12-month trajectories of depression in those reporting
SI and other patients.
"Method
Observational data were available for 3781 patients at
entry to treatment, 2112 at three months and 777 for 12 months. Self-reported
depressed mood and SI were assessed using items from the PHQ-9. Additional data
included sociodemographic characteristics and self-reported well-being.
"Results
25% of the sample reported SI at treatment entry and
those with SI had higher levels of depressed mood (mean = 17.4 vs. 11.3;
F(1,3533) = 716.5, p < .001) and disturbed sleep (mean = 13.8 vs. 12.2,
F(1,3533) = 125.9, p < .001), poorer general health (mean = 43.6 vs. 52.2,
F(1,3533) = 118.3, p < .001) and lower quality of life (mean = 0.44 vs. 0.56
(F(1,3533) = 118.3, p < .001). The prevalence of SI reduced from 23.6% to 17.6%
(z = 6.5, p < .001) at 3 months. Twelve-month follow-up indicated a substantial
reduction in depressed mood with this reduction being more pronounced in those
reporting SI (mean (baseline) = 17.7 vs. mean (12 months) = 10.3) than in other
patients (mean (baseline) = 11.1 vs. mean (12 months) = 7.0).
"Conclusions
SI is common among individuals seeking CBMPs to treat
a range of chronic conditions and is associated with higher levels of depressed
mood and poorer quality of life. Treatment with CBMPs reduced the prevalence and
intensity of suicidal ideation."
https://www.tandfonline.com/doi/10.1080/13811118.2024.2356615?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
[3866]
In "Controlled Inhalation of
Tetrahydrocannabinol-Predominant Cannabis Flos Mitigates Severity of
Post-Traumatic Stress Disorder Symptoms and Improves Quality of Sleep and
General Mood in Cannabis-Experienced UK Civilians: A Real-World, Observational
Study" from Sultan et al (2024):
"Results from this observational study suggest an
association between treatment with THC-predominant cannabis flowers and
symptomatic improvement for up to 6 months in a cohort of UK civilians diagnosed
with PTSD. The treatment was safe and well tolerated and characterized by marked
effects on quality of sleep, general mood, and severity of PTSD-associated
symptoms. Despite previous exposure to cannabis, participants continued to
report benefits after initiating treatment with THC-predominant cannabis
flowers."
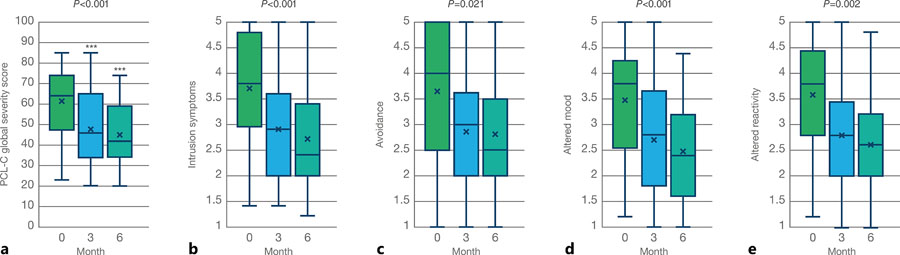
https://karger.com/mca/article/7/1/149/912500/Controlled-Inhalation-of-Tetrahydrocannabinol
[3858]
In "The Effectiveness and Adverse Events of
Cannabidiol and Tetrahydrocannabinol Used in the Treatment of Anxiety Disorders
in a PTSD Subpopulation" (2023) from Stack et al of the University of Sydney's
School of Pharmacology and Applied Cannabis Research in Sydney, NSW, Australia:
"The median doses taken were 50.0 mg/day for CBD and
4.4 mg/day for THC. The total participant sample reported significantly improved
anxiety, depression, fatigue, and ability to take part in social roles and
activities. Those who were diagnosed with PTSD (n = 57) reported significantly
improved anxiety, depression, fatigue, and social abilities. The most common AEs
reported across the whole participant cohort were dry mouth (32.6%), somnolence
(31.3%), and fatigue (18.5%), but incidence varied with different cannabis
formulations. The inclusion of THC in a formulation was significantly associated
with experiencing gastrointestinal AEs; specifically dry mouth and nausea.
Conclusions: Formulations of cannabis significantly improved anxiety,
depression, fatigue, and the ability to participate in social activities in
participants with anxiety disorders. The AEs experienced by participants are
consistent with those in other studies."
And of special note:
"Participants who took a THC-dominant formulation
reported a significant decrease in their anxiety levels. Those same participants
also represented the highest proportion of participants that were classified as
having clinical improvement (61.1%, n = 11), compared with participants who were
prescribed other formulation types. This was unexpected as the median THC dose
for this participant group was 33.8 mg/day, and it has been suggested that doses
higher than 30 mg/day could be anxiogenic. A study reported that doses of CBD
ranging from 15 to 60 mg/day could offset the anxiogenic properties of THC,
which is reflected in our data; however, with lower doses of CBD (median = 6.0
mg/day CBD)."
https://journals.sagepub.com/doi/pdf/10.1177/87551225231180796 [4557]
As assessed by Sultan et al (2024), "Controlled Inhalation of
Tetrahydrocannabinol-Predominant Cannabis Flos Mitigates Severity of
Post-Traumatic Stress Disorder Symptoms and Improves Quality of Sleep and
General Mood in Cannabis-Experienced UK Civilians: A Real-World, Observational
Study"
"Participants were asked to complete the PTSD checklist for civilians (PCL-C).
The PCL-C is a 17-item self-report measure of the 17 DSM-IV symptoms of PTSD.
The PCL-C has a variety of purposes, including screening individuals for PTSD,
diagnosing PTSD, and/or monitoring symptom change during and after treatment.
The PCL-C asks about symptoms in relation to “stressful experiences” and can be
used with any population. The symptoms endorsed may not be specific to just one
event, which can be helpful when assessing survivors who have symptoms due to
multiple events. Furthermore, the 17 items within the PCL-C can be grouped into
the four clusters of symptoms that characterize PTSD: items 1–5 refer to
symptoms of intrusion, questions 6 and 7 capture symptoms of avoidance,
questions 8–12 correspond to symptoms of altered mood, and finally questions
13–17 report symptoms of altered reactivity. Evidence suggests that a 5–10-point
change represents reliable change (i.e., change not due to chance) and a
10–20-point change represents clinically significant change. Therefore, it is
recommended to use 5 points as a threshold for determining whether an individual
has responded to treatment and 10 points as a threshold for determining whether
the improvement is clinically meaningful."
And...
"Fifty-eight patients were included, 34 of which also had PROMs
[patient-reported outcome measures] recorded at 6 months. Most were males
(65.5%) with an average age of 39.2 years who had previously used cannabis
illicitly (95.6%). At 3 months, participants reported significant improvements
in overall health, mood, and sleep quality (p < 0.001) but not in the proxy for
HRQoL (p = 0.052). Similarly, participants reported substantial benefits in
managing intrusion symptoms (p < 0.001), mood alterations (p < 0.001), and
reactivity alterations (p = 0.002), which were sustained or further improved at
6 months. Participants did not report any side effects associated with CBMPs."
https://pmc.ncbi.nlm.nih.gov/articles/PMC11521486/ [4906]
Ma et al (2025) looked at "Involvement of endocannabinoid receptor 1 in
oxidative and inflammatory responses underlying anxiety-like behavior in
SPS&S-exposed mice":
"This study employed the single prolonged stress and shock (SPS&S) model, a
validated rodent paradigm of PTSD, to evaluate the expression of key eCB system
proteins within the medial preftontal cortex (mPFC), Hip, and Amy – brain
regions critically implicated in PTSD pathophysiology (Ressler et al., 2022).
Furthermore, using the systemic administration of the CB1 receptor agonist WIN
55,212-2, we investigated the modulation of CB1 receptor activation on oxidative
stress products, inflammatory responses and PTSD-related behaviors."
...
"SPS&S exposure induced significant anxiety-like behaviors and increased
freezing in fear tests. It decreased CB1 receptor and NAPE-PLD expression while
increasing FAAH and MAGL levels in all examined brain regions, alongside
elevated IL-1β and caspase-1. Plasma oxidative stress and inflammatory cytokines
were also elevated. WIN 55,212-2 administration mitigated anxiety-like behaviors
but not conditioned fear responses. Crucially, it normalized the elevated plasma
oxidative stress and inflammatory cytokine levels."
https://www.sciencedirect.com/science/article/abs/pii/S0014299925008143?via%3Dihub
[5306]
Of THC's endogenous homologue anandamide, Ney and
Matthews (2025) say:
"Posttraumatic stress disorder (PTSD) is characterized
by profound changes to stress systems and impairments in fear extinction, the
process believed to underlie recovery from a traumatic experience. This chapter
reviews the contribution of anandamide—an important endocannabinoid—to human and
animal stress responding as well as fear conditioning with relevance to PTSD.
Anandamide is critical to the activation of the stress response and is
differentially expressed following exposure to trauma. It is also critical to
the extinction of conditional fear and may present a feasible target for
treatment by increasing the capacity for patients to consolidate extinction
memories during exposure therapy."
https://www.sciencedirect.com/science/article/abs/pii/B9780443190810000160
[3859]
Mederos et al (2024) elaborate on the role of the ECS
in "Overwriting an instinct: visual cortex instructs learning to suppress fear
responses":
"Fast instinctive responses to environmental stimuli
can be crucial for survival but are not always optimal. Animals can adapt their
behavior and suppress instinctive reactions, but the neural pathways mediating
such ethologically relevant forms of learning remain unclear. We found that
posterolateral higher visual areas (plHVAs) are crucial for learning to suppress
escapes from innate visual threats through a top-down pathway to the
ventrolateral geniculate nucleus (vLGN). plHVAs are no longer necessary after
learning; instead, the learned behavior relies on plasticity within vLGN
populations that exert inhibitory control over escape responses. vLGN neurons
receiving input from plHVAs enhance their responses to visual threat stimuli
during learning through endocannabinoid-mediated long-term suppression of their
inhibitory inputs. We thus reveal the detailed circuit, cellular, and synaptic
mechanisms underlying experience-dependent suppression of fear responses."
They explain:
"The model exhibited depression of inhibitory synapses
onto vLGN neurons that receive input from plHVAs during learning. Such a form of
synaptic plasticity, called long-term depression of inhibition (iLTD), has been
previously described in multiple brain areas in vitro and is dependent on
endocannabinoid (eCB) signaling. Heterosynaptic iLTD can be triggered by
activation of group I metabotropic glutamate receptors (mGluR1 or mGluR5) in
postsynaptic neurons. This causes release of eCBs which act as retrograde
messengers, activating eCB receptors (CB1R) on nearby presynaptic inhibitory
terminals which can induce a long-lasting reduction of presynaptic GABA release
probability. Allen Institute gene expression data showed that eCB receptor CB1R
and mGluR5 are highly expressed in vLGN (Fig. S7A-B). We therefore investigated
if eCB-dependent iLTD in vLGN could mediate learned suppression of escape."
https://www.biorxiv.org/content/10.1101/2024.07.31.605567v1.full.pdf [4738]
In "Association of the HTR2A 102T/C polymorphism with
attempted suicide: a meta-analysis" Wang et al (2015) concluded:
"Our meta-analysis does not support the previously
suggested association between HTR2A 102T/C and attempted suicide in the general
population. However, in patients with schizophrenia, the C/C genotype of 5-HT2A
receptor 102T/C may increase the risk of attempted suicide."
https://pubmed.ncbi.nlm.nih.gov/26075944/ [4742]
Turiaco et al (2024) ask about the "Genetics of
suicide ideation. A role for inflammation and neuroplasticity?" in the European
Archives of Psychiatry and Clinical Neuroscience:
"Exposure to suicide or suicide attempts increases the
risk of suicidal behavior. One of the strongest clinical predictors of SB is the
non-suicidal self-injury. SI and SB are favored by predisposing risk factors
such as loneliness, hopelessness, demoralization, economics factors, cultural
factors, or social isolation due to belonging to a social minority."
Single-gene theories are now generally debunked.
"SCZ patients with SI have over a six-fold increase of
suicide, while people who had at least one lifetime psychotic event has double
odds of experiencing SI, triple odds of a future suicide attempt, and four times
the odds of dying by suicide. Given those data, the importance of identifying
biological and genetic biomarkers emerges. Our study tried to reach this aim
using a classic GWAS approach, a molecular pathway analysis and modelling the
polygenic risk score with the clinical predictors in a model through machine
learning. No SNP alone reached a GWAS significance in identifying the genetic
risk for SI."
However...
"B3GALTL gene product codes for a protein that is
implicated in synaptogenesis. Quite interestingly, B3GALTL is expressed in the
brain by neurons and astrocytes (proteinatlas.org). It is also expressed in T
cells. This finding is then of particular relevance: Microglia are the primary
immune system cells in the central nervous system, and they function like
peripheral macrophages, releasing a multitude of pro-inflammatory cytokines and
chemokines. Post-mortem examination of suicide patients shows an increased
density of microglia in anterior cingulate cortex, dorsolateral prefrontal
cortex, and mediodorsal thalamus regions. An increased microglial activation is
identified by PET in patients with SI. Microglial cells affect the
tryptophan-kynurenine pathway, increasing the production of neurotoxic
metabolites such as quinolinic acid, a NMDA agonist and creating an imbalance in
the glutamatergic system. Glutamate neurotransmission is the background of a
normal cognitive and emotional processing, so its disruption can lead to
increased impulsivity, depressed mood, and suicidality. Consistently with this
finding, another important molecule involved in neuroinflammation is the 18-kDa
Translocator Protein (TSPO), whose expression was significantly increased in
patients with SI, most robustly in the regions of the anterior cingulate cortex.
Refer to Table 5, for previous relevant studies about schizophrenia,
neuroinflammation and SI."
https://pmc.ncbi.nlm.nih.gov/articles/PMC11422468/ [4743]
Several lines of evidence indicate that abnormalities
in the functioning of the central serotonergic system are involved in the
pathogenesis of depressive illness and suicidal behavior.
https://pubmed.ncbi.nlm.nih.gov/19224112/ [298]
https://pubmed.ncbi.nlm.nih.gov/29526601/ [299]
https://pubmed.ncbi.nlm.nih.gov/11727894/ [300]
Research does not seek to eliminate environmental
influences in favour of genetic disposition in depression, suicidal ideation and
completed suicide. But there are only two hypotheses for the high incidence in
Slovenia, both of which may be right, namely that some are genetically
predisposed to snap when stress is prolonged or reaches a certain level, or that
living conditions for some, according to the rules constructed by their own
society, are relentlessly sub-optimal.
Slovenia is an ideal candidate for psychedelic
therapy. Slovenia ruminates endlessly about the past. Millions of tonnes of CO2
are expended generating hot air about long-dead regimes and ideologies, because
they have affected people in this area. But arguing about what Tito wrote about
Stalin in 1940 won't bring your dead relatives back or make you happy and strong
today. To ignore the past and bury the hatchet seems like a cop-out. But the
past is getting in the way of the present, and the future.
"In 1976, a man known as Ka-Tzetnik 135633 (original
name: Yehiel De-Nur) underwent LSD-assisted psychotherapy. At the time, he was
under the supervision of Prof. Jan Bastiaans at the State University of Leiden
in the Netherlands. Bastiaans was the psychiatrist who had first identified
concentration camp syndrome, also known as survivor syndrome. This syndrome is a
form of what we would now call post-traumatic stress disorder (PTSD). Its
characteristics include social withdrawal, sleep disturbance, anxiety, and
depression. Bastiaans had also successfully treated this syndrome with
LSD-assisted psychotherapy. Ka-Tzetnik 135633 was a survivor of Auschwitz, where
he was a prisoner for two years. This trauma was followed by three decades of
torment, in which he relived the horror of those two years at night. Through
LSD-assisted psychotherapy, however, Ka-Tzetnik 135633 found healing.
"Almost a half century after Bastiaans' successful
trials, the regulation of psychedelics for treating PTSD is finally underway.
Think of the Holocaust survivors who might have found healing through these
medicines, but couldn't because of a politically-motivated ban on psychedelics.
This realization brings home the horrific impact of the failed war on drugs.'"
https://realitysandwich.com/psychedelics-and-judaism/ [1092]
Many diagnosed with PTSD are unimpressed by the medical response. Modlin et al
(2025) report on self-treatment strategies: cannabis and psychedelics were the
two most preferred, with MDMA a close third:
"An online survey recruited individuals with self-reported trauma symptoms or a
formal diagnosis of post-traumatic stress disorder (PTSD)/complex post-traumatic
stress disorder (CPTSD). Participants were asked about their treatment history,
satisfaction with current treatments, and use of illicit substances for symptom
management. Further, after receiving psychoeducation on
3,4-methylenedioxymethamphetamine (MDMA) and psilocybin therapies, participants’
perceptions and willingness to participate in these treatments were assessed.
"Results: Of the 873 respondents, 94.8% reported experiencing psychological
trauma, with 73.4% diagnosed with PTSD or CPTSD. Many had attempted multiple
treatments, predominantly medications and various psychotherapies, but reported
high dissatisfaction. Significant rates of marijuana, psychedelics, and MDMA use
for self-management of trauma symptoms were reported, with minimal physical and
psychological complications. Willingness to try MDMA and psilocybin therapies
was high (0.81 and 0.83, respectively). Notably, women and heterosexual
individuals showed lower willingness, while younger respondents and those with
higher education levels showed greater willingness to try these treatments.
"Conclusion: High willingness to try MDMA and psilocybin therapies among
trauma-exposed individuals highlights the need for further research and clinical
trials. Understanding demographic variations in willingness can guide the
development of accessible and effective treatment options for PTSD and CPTSD.
Public education about potential risks and harm reduction strategies is crucial
to promote safe and informed use of these emerging therapies."
https://psychiatry-psychopharmacology.com/Content/files/sayilar/142/S3-S19.pdf
[5365]
Psychedelics break the rumination cycle by disrupting
- in a good way - brain activities which perpetuate habitual thinking and
behaviour.
The most abundant 5-HT receptors expressed in the
medial prefrontal cortex (mPFC) are 5-HT1AR and 5-HT2AR. The 5-HT2AR pathway is
enhanced by 5-HT2AR-agonist psychedelics.
https://pubmed.ncbi.nlm.nih.gov/28858536/ [301]
In mice, given a single dose of psilocybin or LSD, and
using the social reward conditioned place preference (sCPP) assay Nardou et al
have made an important step forward in understanding the mechanism by which
psychedelics can override cultural log-jams retarding progress and societal
happiness, such as we see in Slovenia. "Psychedelics reopen the social reward
learning critical period" (2023) finds:
"Psychedelics are a broad class of drugs defined by
their ability to induce an altered state of consciousness. These drugs have been
used for millennia in both spiritual and medicinal contexts, and a number of
recent clinical successes have spurred a renewed interest in developing
psychedelic therapies. Nevertheless, a unifying mechanism that can account for
these shared phenomenological and therapeutic properties remains unknown. Here
we demonstrate in mice that the ability to reopen the social reward learning
critical period is a shared property across psychedelic drugs. Notably, the time
course of critical period reopening is proportional to the duration of acute
subjective effects reported in humans. Furthermore, the ability to reinstate
social reward learning in adulthood is paralleled by metaplastic restoration of
oxytocin-mediated long-term depression in the nucleus accumbens. Finally,
identification of differentially expressed genes in the ‘open state’ versus the
‘closed state’ provides evidence that reorganization of the extracellular matrix
is a common downstream mechanism underlying psychedelic drug-mediated critical
period reopening. Together these results have important implications for the
implementation of psychedelics in clinical practice, as well as the design of
novel compounds for the treatment of neuropsychiatric disease."
https://www.nature.com/articles/s41586-023-06204-3 [2825]
But we do not need to rely on mice when there are
real-life mass traumas going on. A special opportunity came along on 7 October
2023 in the Hamas attack on Supernova. "Trauma Under Psychedelics: MDMA Shows
Protective Effects During the Peritraumatic Period" say Netzer et al (2024):
"Traumatic events (TEs) play a causal role in the
etiology of psychopathologies such as depression and posttraumatic stress
disorder (PTSD). Recent research has highlighted the therapeutic potential of
psychoactive substances and especially 3,4-methylenedioxymethamphetamine (MDMA),
in alleviating trauma symptoms in chronic patients. However, little is known
regarding the consequences of trauma that is acutely experienced under the
influence of psychoactive substances. Here we investigated the acute experiences
and peritraumatic processing of 657 survivors from the high-casualty terror
attack at the Supernova music festival in Israel on October 7th, 2023. Data were
collected four to twelve weeks following the TE. Approximately two-thirds of
survivors were under the influence of psychoactive substances at the time of the
TE, offering a tragic and unique natural experiment on the impact of
psychoactive compounds on TE processing. Our findings reveal that individuals
who experienced the trauma while under the influence of MDMA demonstrated
significantly improved intermediate outcomes compared to those who were under
the influence of other substances or no substances at all. Specifically, the
MDMA group reported increased feelings of social support, more social
interactions and enhanced quality of sleep during the peritraumatic period,
yielding reduced levels of mental distress and reduced PTSD symptom severity.
These novel findings suggest that the influence of MDMA during the TE may carry
protective effects into the peritraumatic period, possibly mediated through the
known effects of MDMA in reducing negative emotions and elevating prosociality.
These protective effects in turn may mitigate the development of early
psychopathology-related symptoms. Current preliminary results underscore the
need for further understanding of the cognitive and physiological processes by
which psychedelic substances intersect with trauma recovery processes."
https://www.biorxiv.org/content/10.1101/2024.03.28.587237v1 [3174]
With "Facing trauma under the influence of psychedelics: A phenomenological
study with Nova rave survivors" psychedelic research found a new angle. Two
thirds of the Israeli festivalgoers attacked On 7 October 2023 were under the
influence of LSD, mushrooms, ketamine or MDMA, say Simon et al (2025):
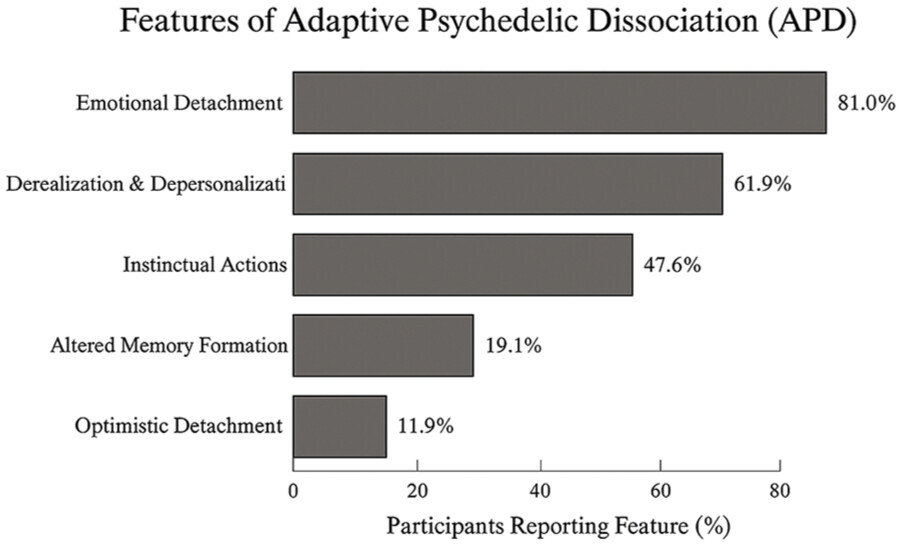
"Participants’ awareness and knowledge about their substance use created an
'epistemic container,' which may have facilitated real-time containment of
traumatic input while complicating later meaning-making. A neurophenomenological
pattern emerged wherein psychedelic subjective effects appeared suppressed
during the acute trauma exposure, resurging after the threat was over.
Quantitative analysis showed a predominantly positive subjective impact of
substance use on immediate survival (75%–79%) and emotional coping (83%–84%) but
mixed outcomes in aftermath processing (42%–53% positive and 25%–26% negative).
"Conclusions:
Psychedelic-induced dissociation during trauma exposure may confer acute
adaptive benefits while causing integration challenges a paradox with
significant implications on trauma research. This singular perspective on the
psychedelic–trauma interface invites further research into these complex
neuropsychological interactions. Psychedelics may serve as epistemological
instruments, revealing cognitive processes and unique prisms through which
trauma response, psychopathology, resilience, and the adaptive capacities of the
human mind under extreme conditions can be re-examined."
Unfortunately evaded in this "unique interaction between psychedelic states and
extreme stress" (a description suggesting the authors have not studied tripping
in Lincoln on a Saturday night) was the opportunity to include a control group.
So the chances of comparing survival rates and other parameters between users
and non-users have been lost.
With this methodology there was no danger of demonstrating evolutionary
advantages of elevated consciousness, although the authors findings suggest
exactly this: psychedelics use "seems to have created a distinct form of
psychological protection that both aided immediate survival and posed challenges
for later integration".
"Optimistic detachment" helped users to cope with the threat and being sharp
enabled them to act smart.
How to help never-users understand this? In support of the Defence claim that
the ZPPPD as it applies to psychedelics (excluding ketamine and MDMA) is an
unconstitutional restriction of evolutionary advantage, the Defendant compares
the value of psychedelics amid stressful conditions to the "unconscious
competence" of driving a vehicle normally (second-nature behaviour,
background-task capable), as opposed to sweating neurotically over every control
movement.
As for any increased difficulties in the aftermath, you remember the last book
you read, but are unlikely to recall any specific text. You won't have to worry
about PTSD recovery later if you are dead. If you have more information to
integrate, chances are the result will be more integrated.
Once again, the opportunity to compare recovery patterns between psychedelic and
non-users with controls was eluded rather than elucidated in this, perhaps the
ultimate survivor-biased study. Perhaps the other third of the festivalgoers
couldn't be found.
https://journals.sagepub.com/doi/10.1177/02698811251372508?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
[5651]
As of 2025 no comparison of survival by drug type at Supernova pertains.
However, the Court must hear that it is more bad news for any followers of
Slovenian culture who find themselves under attack as, following a study by
Nacasch et al (2025):
"The team hypothesised that survivors who were on drugs at the time would have
been more hyper-aware of the event and their surroundings, thereby experiencing
more post/trauma from the attack overall. However, they were wrong."
Unfortunately for Slovenia's majority drug-choosers:
"'It was the alcohol,' [Professor Mark Weiser] told Health Policy Watch. 'These
people were the ones who had more severe post-traumatic symptoms.'"
https://healthpolicy-watch.news/study-alcohol-not-psychedelics-linked-to-heightened-trauma-in-survivors-of-attack-on-israeli-festival-goers/
[5652]
Note: this was one of those occasions when alcohol wasn't a "drug".
"Seventy-one of them (57.7%) reported using psychoactive drugs at the festival –
12 only alcohol, nine only lysergic acid (LSD), seven only
3,4-methylenedioxymethamphetamine (MDMA), six only cannabis, three only
methylmethcathinone (MMC), 15 various drug combinations including alcohol, and
19 various drug combinations excluding alcohol."
Despite all the harmful illegality adding to the background stress, the
pro-alcohol researchers had to admit defeat:
"The multiple regression analysis of the PDEQ [Peritraumatic Dissociative
Experiences Questionnaire] dissociation score with VAS-A [Visual Analog Scale
for Anxiety], GAD-7 [Generalized Anxiety Disorder-7], PHQ-9 [(Patient Health
Questionnaire-9], and PDS-5 [Posttraumatic Diagnostic Scale] subscale scores,
including gender and age, was statistically significant (p=0.0001)."
Each of the component scores were also statistically significant except VAS-A.
In more great news for the nation's psychiatrists and pharma concerns...
"...in marked contrast to our expectations, we found that only pre-trauma
alcohol consumption, with or without other drugs, significantly increased the
risk of peri-traumatic dissociation, anxiety,depression, and ASD [acute stress
disorder] symptoms."
https://onlinelibrary.wiley.com/doi/pdf/10.1002/wps.21254 [5653]
Another alternative to mice is "Human pluripotent stem
cells as a translational toolkit in psychedelic research in vitro". As Salerno
and Rehan explain:
"PSCs can differentiate into various brain cell types,
mirroring endogenous expression patterns and cell identities to recreate disease
phenotypes. Brain organoids derived from PSCs resemble cell diversity and
patterning, while region-specific organoids simulate circuit-level phenotypes.
PSC-based models hold significant promise to illuminate the cellular and
molecular substrates of psychedelic-induced phenotypic recovery in
neuropsychiatric disorders."
and
"The identities of the signaling pathways responsible
for psychedelics’ hallucinogenic and therapeutic properties and whether these
are distinct or overlapping pathways are some of the questions still under
debate.
"The Gq or β-arrestin-2 recruitment paradigm
represents a glimpse into the extensive network of pathways regulated by 5-HT2AR
activation via psychedelics. For example, distinct psychedelics activate
phospholipase A2 and phospholipase D via ADP-ribosylation factor 1. The
activation of 5-HT2AR, triggered by various agonists including DOI and LSD, can
lead to the heterodimerization of the receptor with metabotropic glutamate
receptor 2 and dopamine D2 receptor, both of which are Gi-coupled receptors.
This transactivation blocks the cAMP’s synthesis by adenylate cyclase and
prompts heterotrimeric Gi/o proteins to trigger Src-mediated downstream events.
"A burst of glutamate also follows psychedelic
administration, mainly in the cortical layer V of the neocortex, which is a
5-HT2AR-enriched area.8,23 High glutamate levels activate the
α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR), boosting
the secretion of brain-derived neurotrophic factor (BDNF), which in turn signals
through the tyrosine receptor kinase B (TrkB) and mammalian target of rapamycin
(mTOR) pathways, sustaining both the AMPAR activation and BDNF secretion in a
positive feedback loop of neural plasticity.
"Furthermore, the hallucinogenic properties of
different psychedelics are also proposed to be influenced by other 5-HTRs, and
not all 5-HT2AR agonists have hallucinogenic properties. For instance, human
studies also provide evidence supporting the involvement of the 5-HT1AR in the
effects of psilocybin. Competition binding studies on rodent brains and primary
cells revealed a lack of pronounced selectivity of psilocin for 5-HT2AR over
5-HT1AR. Nevertheless, the role of the 5-HT2AR remains the subject of more
extensive study and investigation. Ketanserin, a selective antagonist of the
5-HT2Rs, effectively eliminates head-twitch behavioral responses in mice;
however, it does not attenuate psilocybin-induced structural modifications in
the prefrontal cortex. As a result, uncertainties remain about whether and how
the neuroplastic effects on rescuing disease phenotypes relate to behavioral
responses, especially in humans. Moreover, human studies investigating the
molecular mechanisms of psychedelic-induced plasticity rely on global parameters
such as peripheral BDNF levels, which may not correlate with the molecular
mechanisms occurring in brain cells. For in-depth cellular and molecular
insights into the role of 5-HT2AR, in vitro investigations are required."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11019282/ [3173]
Using PSCs Schmidt et al (2024) of the University of
Heidelberg showed that psilocin causes 5-HT2A receptor internalization and
redistribution in human cortical neurons, induces BDNF expression and downstream
signaling in human neurons in a dose-dependent manner, induces gene expression
changes associated with axonal and synaptic plasticity, increases dendritic
complexity, and increases synaptic strength and synaptogenesis.
https://www.researchgate.net/publication/381253376_Psilocin_fosters_neuroplasticity_in_iPSC-derived_human_cortical_neurons
[3175]
Blest-Hopley et al (2025) found "improved mental
health outcomes and normalised spontaneous EEG activity in veterans reporting a
history of traumatic brain injuries following participation in a psilocybin
retreat":
"This study investigates the effects of psilocybin
administered in retreat settings on veterans with a history of TBI, focusing on
mental health outcomes and changes in brain connectivity as measured by EEG.
"Methods: A total of 21 participants were recruited
through the Heroic Hearts Project, which facilitated access to two six-day
psilocybin retreats in Jamaica. Before the retreat, participants underwent three
individual and three group coaching sessions to prepare for the experience.
During the retreat, two psilocybin ceremonies were held, spaced 48 hours apart.
Participants received an initial dose of 1.5g to 3.5g of dried psilocybin
mushrooms, with the option to increase the second dose up to 5g. Psilocybin was
administered in a tea format, under the supervision of experienced facilitators.
Psychological outcomes were assessed using validated questionnaires (PCL-5,
PHQ-9, STAI) at baseline (four weeks pre-retreat) and four weeks post-retreat.
Electroencephalography (EEG) was used to measure brainwave activity pre- and
post-treatment. Paired t-tests were used to analyze changes in psychological
scores, while EEG frequency band analysis assessed changes in brain function and
connectivity.
"Results: Improvements were observed across several
mental health measures: PTSD (PCL-5 scores decreased by 50%, p=0.010),
depression (PHQ-9 scores decreased by 65%, p<0.001), and anxiety (STAI) scores
decreased by 28%, p<0.001). EEG data showed decreased delta and theta power in
frontal and temporal regions, indicating potential improvements in cognitive
control and emotional processing. Enhanced coherence in alpha and beta bands
suggested improved neural communication."
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1594307/full
[5324]
Administration of psychedelics to a relatively small
number of people could bring the paralysing stand-off over Slovenia's past to a
quick and elegant halt. The participants would see the damage they are doing -
to themselves and the country - by perpetuating hostilities against groups and
against individuals long dead. They would be able to more accurately gauge the
importance of the historical against the challenges of the present and future.
They would be less susceptible to fearmongering and superstition. Their
nightmares would be put into perspective.
The Slovenians who stand to gain the most from ranting
on about the past for political purposes are the least likely to have taken
them. Among them you will find the most enthusiastic opponents of the benefits
of psychedelics, about which their ignorance resembles what the average villager
in Radenci knows of Tito in the 1940s, i.e. what they have been told, not what
they have experienced.
Unnecessary and counterproductive rigidity are legal
and mental constructs that can be ameliorated by mind-expanding drugs. They
offer a sideways view, and offer users the opportunity to invite unnecessary and
counterproductive rigidity to get lost. And this is why the anti-drug religion,
prohibition, doesn't like them.
Oblivion from alcohol, often associated with violence,
is a legally approved coping mechanism, but is solipsistic and does nothing to
solve the underlying malaises. Drugs other than alcohol, which can give rise to
creative solutions to life stresses or at least relief by way of euphoria are
legally disapproved, and the users accused of escapism. A drug user is not
concerned with his or her genetic predisposition. They can't change that.
What Slovenia's warring factions need is not more
press stories about what the communists did, but consolation now. Now does not
contain the grudges of the past, nor the anxieties of the future. Now is not a
popular concept for political manipulators. "Now" suggests something should be
done, rather than talked about. "Now" cannot play on people's resentments and
fears. Dealing with "Now" may be financially expensive compared to promises and
grumbling.
Although it is not necessary to understand the
mechanisms of the human brain by which consolation takes place, and psychedelic
people have managed without this so far, it's good to know the scientists are
finally being allowed to fill in the details, and the activation of 5-HT1A
receptors in the anterior cingulate cortex was sufficient to reverse consolation
and sociability deficits in Chinese mandarin voles.
https://elifesciences.org/articles/67638 [302]
I think it might work in Slovenians too.
From "The Role of Nutrients in Protecting
Mitochondrial Function and
Neurotransmitter Signaling: Implications for the
Treatment of
Depression, PTSD, and Suicidal Behaviors" by Du et al
(2016):
"Drugs, which lower the cholesterol levels, are able
to cause the depressive symptoms (Tatley and Savage, 2007). In addition,
fish-intake (rich in EPA or DHA) directly protects against the onset of major
depressive disorder (Weidner et.al., 1992). Moreover, chronic stress induced an
inhibition to the respiratory chain in the mitochondria in the brain (Madrigal
et al., 2001). Mitochondrial dysfunction caused by changes in biochemical
cascade or the damage to the mitochondrial electron transport chain has been
suggested to be an important pathogenic factor for the psychiatric disorders,
particularly in bipolar disorders and depression (Rezin et al., 2009). Moreover,
food supplements, such as B12 or folate, which protects mitochondrial functions
are effective as an adjunctive therapy for the treatment of depression
(Papakostas et al., 2005). All these studies imply that mitochondrial
dysfunction and reduced formation of lipid raft may be involved in the etiology
of depression and suicidal behavior (Figure 1). These stress-induced neuronal
dysfunctions interact with the other genetic and environmental factors,
including adverse childhood events, exposure to trauma, drug abuse, smoking,
alcohol usage, sleep, diet, and exercise levels, to precipitate mood disorders
in genetically and/or physiologically vulnerable or predisposed individuals
(Figure 1)."
As for suicide:
"Epidemiological studies have identified low fish
(high in ω-3 fatty acid) consumption as a risk factor for mortality from suicide
(Hibbeln and Salem, 1995, Hirayama, 1990, Sublette et al., 2006, Tanskanen et
al., 2001). One study noted that frequent fish consumption (twice per week or
more) significantly reduced the risk of depressive symptoms and of self-reported
suicidal ideation (Tanskanen et al., 2001). A 17-year follow-up study of over
250,000 Japanese subjects showed that people who ate fish daily had a lower risk
of death from suicide (Hirayama 1990). In addition, several reports indicate
that lower ω3-fatty-acid levels, including lower plasma EPA, and DHA, or EPA in
red blood cells, predicted greater risk of suicide attempt (Hibbeln and Salem,
1995, Huan et al., 2004, Sublette et al., 2006). Because both cholesterol and
DHA are major components of the lipid raft, it is possible that reduced
cholesterol and ω3-fatty-acid levels may affect the formation of lipid rafts in
the CNS, and subsequently reduce neurotransmitter signaling (Czysz and Rasenick,
2013). Notably, increased formation of lipid rafts in the membrane would
facilitate serotonergic (Donati et al., 2008, Renner et al., 2007), dopaminergic
(Villar et al., 2009), and glutamatergic (Francesconi et al., 2009, Ponce et
al., 2008) neurotransmitter signaling; all of these play important roles in the
pathophysiology and treatment of psychiatric disorders. Studies have noted that
low cholesterol levels are associated with increased risk of suicide (Neaton et
al., 1992) and that this association shows an inverse relationship with baseline
total serum cholesterol (Lester, 2002, Lindberg et al., 1992). Other studies
found that individuals who attempted suicide had significantly lower cholesterol
levels than controls (Atmaca et al., 2002, Boston et al., 1996, Kim et al.,
2002, Kunugi et al., 1997, Maes et al., 1997a, Modai et al., 1994,
Rabe-Jablonska and Poprawska, 2000, Sarchiapone et al., 2001, Takei et al.,
1994). A postmortem study found that the brains of violent suicide completers
had a lower grey-matter cholesterol content (Lalovic et al., 2007), and that a
family history of suicidal behavior was more frequent among carriers of
Smith–Lemli–Opitz syndrome, an autosomal recessive disorder characterized by
abnormally low cholesterol levels (Lalovic et al., 2004)."
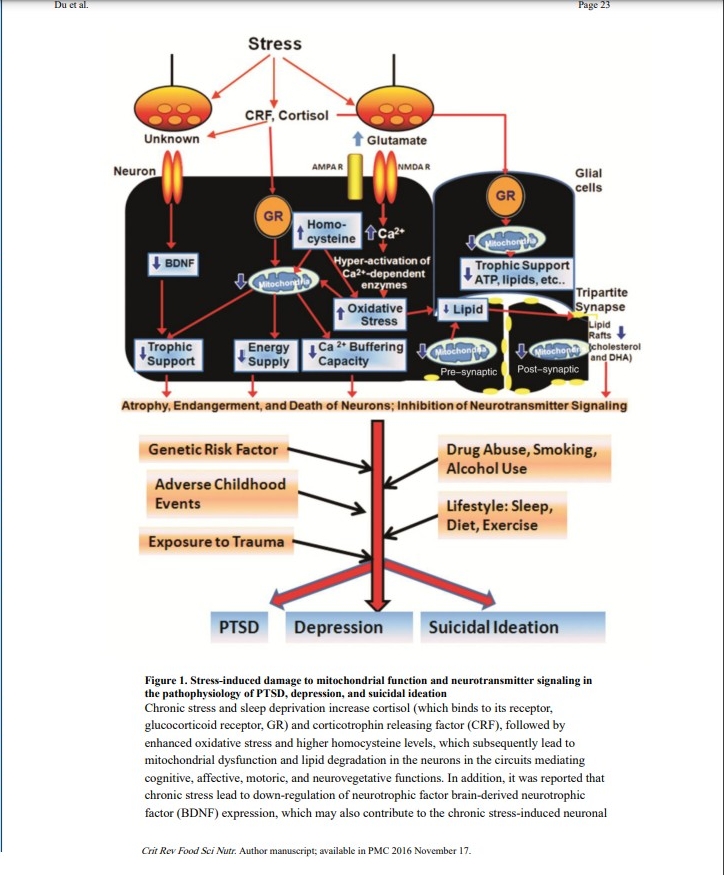
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC4417658&blobtype=pdf
[1817]
By 2023, Song et al's highlights were
"Mitochondrial dysfunction plays a vital role in the
etiology of depression.
Dysregulation of the mitochondrial quality control
system exacerbates the pathophysiology of depression.
Mitochondrial energy metabolism disorders fail to
provide physiological support for neuroplasticity in depression.
The interaction between defective mitochondria and
neuroinflammation worsens depression.
Mitochondria represent a potential target for
pharmacological intervention of depression."
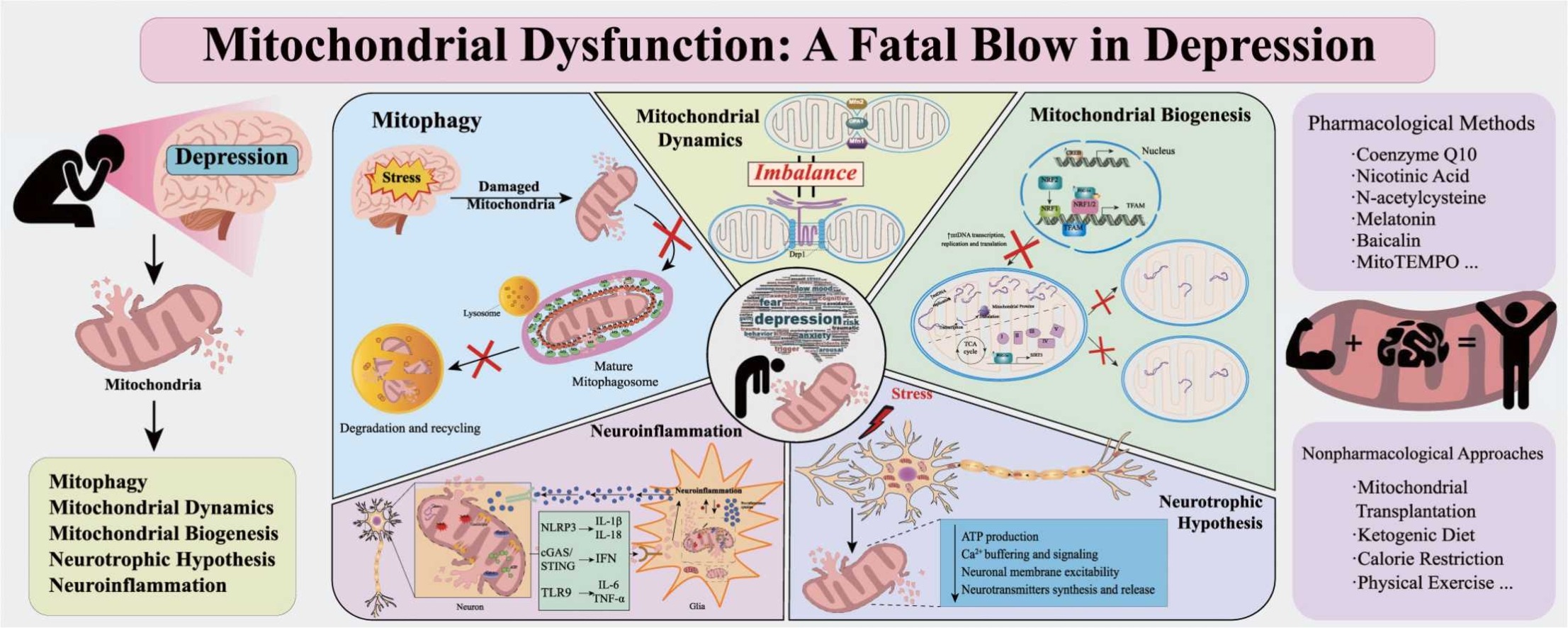
We are reminded:
"BDNF, a substance released by the nerve growth factor
family, known as neurotrophins, controls neuronal survival, preserves neuronal
function and synaptic plasticity, and promotes the synthesis and release of
neurotransmitters . BDNF plays a neuroprotective role by increasing the
respiratory control index via the mitogen-activated protein kinase (MEK)/Bcl2.
Therefore, suppression of the Bcl2-related signaling pathway reduces BDNF
levels, which consequently affects mitochondrial function, resulting in the
impairment of plasticity and initiation of apoptosis. In addition to
manufacturing oxygen and nitrogen species for synaptic plasticity, mitochondria
trigger caspases in dendrites to eliminate postsynaptic spines associated with
chronic depression. In line with mitochondrial function, BDNF enhances the
utilization ratio of oxidation to enable neuronal plasticity."
https://www.sciencedirect.com/science/article/pii/S0753332223014506 [3998]
According to a 2020 review in BMC Psychiatry by
Raymundi et al at the Federal University of Parana in Brazil:
"At low doses, THC can enhance the extinction rate and
reduce anxiety responses. Both effects involve the activation of cannabinoid
type-1 receptors in discrete components of the corticolimbic circuitry, which
could counterbalance the low 'endocannabinoid tonus' reported in PTSD patients.
The advantage of associating CBD with THC to attenuate anxiety while minimizing
the potential psychotic or anxiogenic effect produced by high doses of THC has
been reported. The effects of THC either alone or combined with CBD on aversive
memory reconsolidation, however, are still unknown.
"Conclusions: Current evidence from healthy humans and
PTSD patients supports the THC value to suppress anxiety and aversive memory
expression without producing significant adverse effects if used in low doses or
when associated with CBD. Future studies are guaranteed to address open
questions related to their dose ratios, administration routes, pharmacokinetic
interactions, sex-dependent differences, and prolonged efficacy."
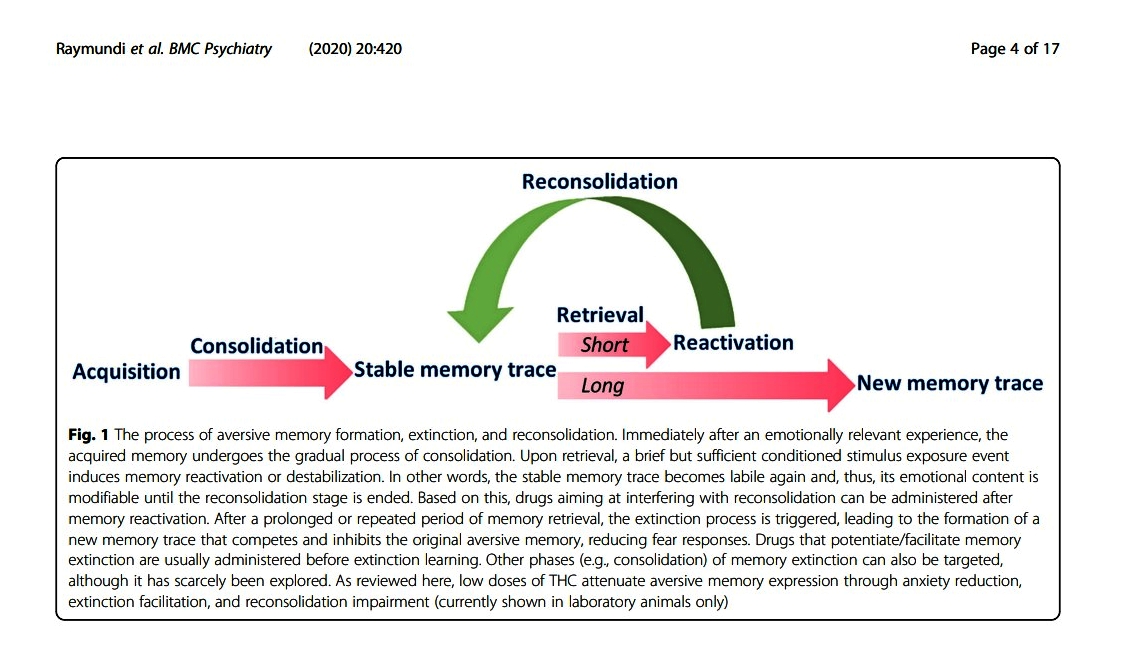
"As reviewed here, low doses of THC attenuate aversive
memory expression through anxiety reduction, extinction facilitation, and
reconsolidation impairment (currently shown in laboratory animals only."
https://bmcpsychiatry.biomedcentral.com/counter/pdf/10.1186/s12888-020-02813-8.pdf
[1506]
By 1985 Howlett had shown "Cannabinoid inhibition of
adenylate cyclase. Biochemistry of the response in neuroblastoma cell
membranes". The fight-or-flight response, which is triggered by adrenaline,
relies on cAMP signaling to increase heart rate and mobilize energy stores. This
system is hyperactive and triggered too easily in PTSD. Inhibiting adenylyl
cyclase would impair this response.
https://chemport-n.cas.org//chemport-n/?APP=ftslink&action=reflink&origin=npg&version=1.0&coi=1%3ACAS%3A528%3ADyaL2MXhvFOqsL0%3D&md5=49106efb644a6fc89de96c071d7d766b
[3731]
By 1997 Glass et al had shown using receptor
audioradiography that
"...cannabinoid receptor binding sites in the human
brain are localized mainly in: forebrain areas associated with higher cognitive
functions; forebrain, midbrain and hindbrain areas associated with the control
of movement; and in hindbrain areas associated with the control of motor and
sensory functions of the autonomic nervous system."
https://pubmed.ncbi.nlm.nih.gov/9472392/ [3729]
Marsicano et al published "The endogenous cannabinoid
system controls extinction of aversive memories" in 2002:
"Acquisition and storage of aversive memories is one
of the basic principles of central nervous systems throughout the animal
kingdom. In the absence of reinforcement, the resulting behavioural response
will gradually diminish to be finally extinct. Despite the importance of
extinction, its cellular mechanisms are largely unknown. The cannabinoid
receptor 1 (CB1) and endocannabinoids are present in memory-related brain areas
and modulate memory. Here we show that the endogenous cannabinoid system has a
central function in extinction of aversive memories. CB1-deficient mice showed
strongly impaired short-term and long-term extinction in auditory
fear-conditioning tests, with unaffected memory acquisition and consolidation.
Treatment of wild-type mice with the CB1 antagonist SR141716A mimicked the
phenotype of CB1-deficient mice, revealing that CB1 is required at the moment of
memory extinction. Consistently, tone presentation during extinction trials
resulted in elevated levels of endocannabinoids in the basolateral amygdala
complex, a region known to control extinction of aversive memories. In the
basolateral amygdala, endocannabinoids and CB1 were crucially involved in
long-term depression of GABA (gamma-aminobutyric acid)-mediated inhibitory
currents. We propose that endocannabinoids facilitate extinction of aversive
memories through their selective inhibitory effects on local inhibitory networks
in the amygdala."
https://pubmed.ncbi.nlm.nih.gov/12152079/ [3730]
With understanding of the glucocorticoid mechanism in
mammals somewhat stuck, in 2003 Di et al revealed "Nongenomic Glucocorticoid
Inhibition via Endocannabinoid
Release in the Hypothalamus: A Fast Feedback
Mechanism":
"The glucocorticoid effect was not blocked by the
nitric oxide synthesis antagonist NG -nitro-L-arginine methyl ester
hydrochloride or by hemoglobin but was blocked completely by the CB1 cannabinoid
receptor antagonists AM251
[N-(piperidin-1-yl)-5-(4-iodophenyl)-1-(2,4-dichlorophenyl)-
4-methyl-1H-pyrazole-3-carboxamide] and AM281
[1-(2,4-dichlorophenyl)-5-(4-iodophenyl)-4-methyl-N-4-morpholinyl-1H-pyrazole3-carboxamide]
and mimicked and occluded by the cannabinoid receptor agonist WIN55,212-2 [( )-(
)-[2,3-dihydro-5-methyl-3-(4-
morpholinylmethyl)pyrrolo[1,2,3-de]-1,4-benzoxazin-6-yl]-1-naphthalenylmethanone
mesylate], indicating that it was mediated by retrograde endocannabinoid
release."
https://www.jneurosci.org/content/jneuro/23/12/4850.full.pdf [3733]
In 2009 new light was shed on the rapid effects of
glucocorticoids in mammals by revealing a putative nongenomic role of
glucocorticoids in regulating emotional learning in rodents through a
coordinated induction of endocannabinoid signaling. Campolongo et al showed
"Endocannabinoids in the rat basolateral amygdala enhance memory consolidation
and enable glucocorticoid modulation of memory":
"Extensive evidence indicates that the basolateral
complex of the amygdala (BLA) modulates the consolidation of memories for
emotionally arousing experiences, an effect that involves the activation of the
glucocorticoid system. Because the BLA expresses high densities of cannabinoid
CB1 receptors, the present experiments investigated whether the endocannabinoid
system in the BLA influences memory consolidation and whether glucocorticoids
interact with this system. The CB1 receptor agonist WIN55,212-2 (5–50 ng per 0.2
μL per side), infused bilaterally into the BLA of male Sprague–Dawley rats
immediately after inhibitory avoidance training, induced dose-dependent
enhancement of 48-h retention. Conversely, the CB1 receptor antagonist AM251
(0.07–0.28 ng per 0.2 μL per side) administered after training into the BLA
induced inhibitory avoidance retention impairment. Furthermore, intra-BLA
infusions of a low and nonimpairing dose of AM251 (0.14 ng per 0.2 μL per side)
blocked the memory enhancement induced by concurrent administration of
WIN55,212-2. Delayed infusions of WIN55,212-2 or AM251 administered into the BLA
3 h after training or immediate posttraining infusions of these drugs into the
adjacent central amygdala did not significantly alter retention performance.
Last, intra-BLA infusions of a low and otherwise nonimpairing dose of AM251
(0.14 ng per 0.2 μL per side) blocked the memory-enhancing effect induced by
systemic administration of corticosterone (3 mg/kg, s.c.). These findings
indicate that endocannabinoids in the BLA enhance memory consolidation and
suggest that CB1 activity within this brain region is required for enabling
glucocorticoid effects on memory consolidation enhancement."
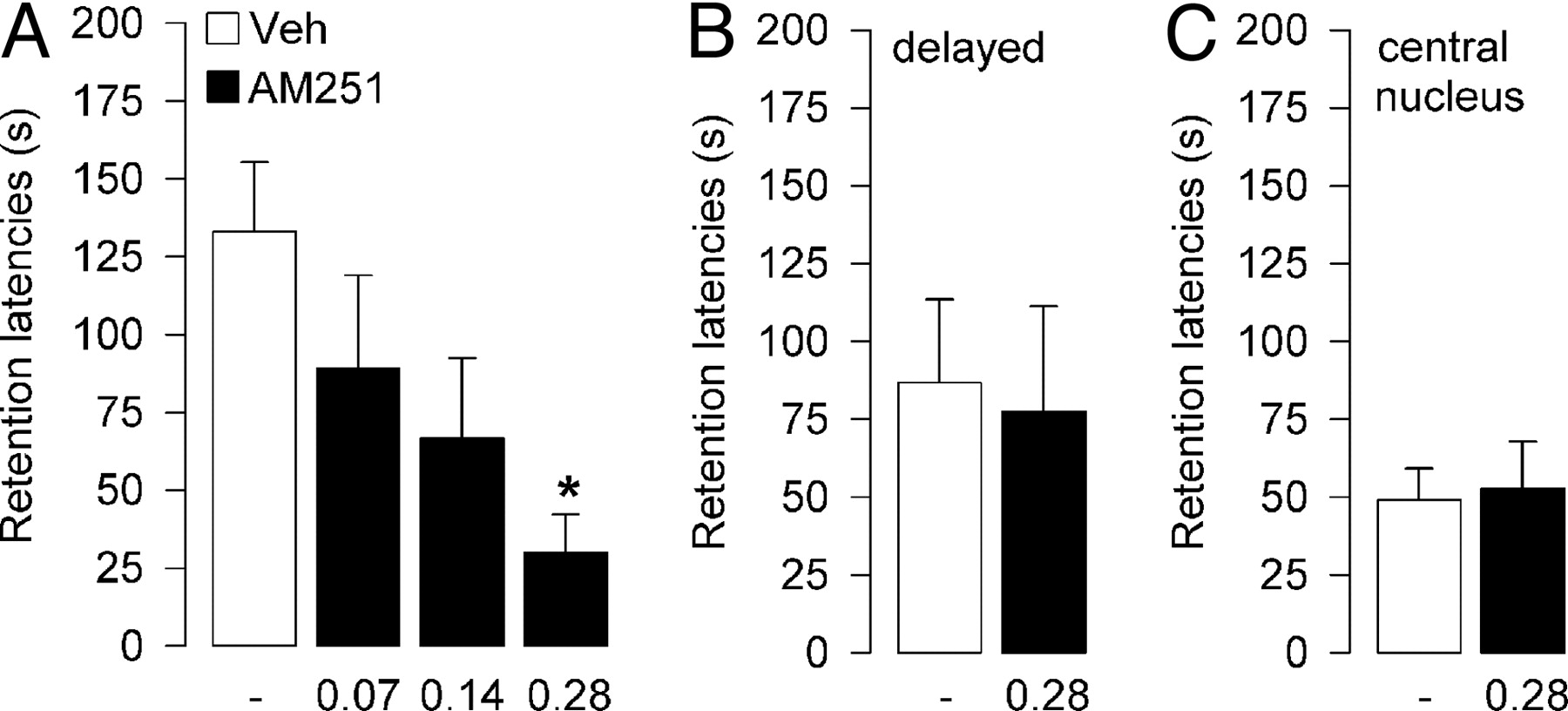
https://www.pnas.org/doi/10.1073/pnas.0900835106 [3732]
In "Cannabinoid modulation of corticolimbic activation
to threat in trauma-exposed adults: a preliminary study" (2020) Rabinak et al at
Wayne State University in Detroit, explained:
"Excessive fear and anxiety, coupled with
corticolimbic dysfunction, are core features of stress- and trauma-related
psychopathology, such as posttraumatic stress disorder (PTSD). Interestingly,
low doses of Δ9-tetrahydrocannabinol (THC) can produce anxiolytic effects,
reduce threat-related amygdala activation, and enhance functional coupling
between the amygdala and medial prefrontal cortex and adjacent rostral cingulate
cortex (mPFC/rACC) during threat processing in healthy adults. Together, these
findings suggest the cannabinoid system as a potential pharmacological target in
the treatment of excess fear and anxiety. However, the effects of THC on
corticolimbic functioning in response to threat have not be investigated in
adults with trauma-related psychopathology."
The results of their fMRI study of 71 human subjects
undergoing a well-established threat processing paradigm demonstrated that:
"In adults with PTSD, THC lowered threat-related
amygdala reactivity, increased mPFC activation during threat, and increased
mPFC-amygdala functional coupling."
...which suggests that
"THC modulates threat-related processing in
trauma-exposed individuals with PTSD..."
Taking fear and happiness as opposing states, the
Defence applauds the astonishing diligence with which scientists are working
towards the discovery of what cannabis users already know: it helps you relax,
reduces rumination, and makes you happy. These detailed, tiny steps are
important. But the backstory does not predate the legally relevant ordinances of
international cannabis control. This provides no useful result today for the
PTSD victim or recreational user, for whom these effects are as intuitively
obvious as those of coffee and do not require scientific proof or peer review.
"Interestingly, CB1Rs are highly abundant in these
regions of the corticolimbic system (Tsou et al. 1998; Marsicano and Lutz 1999;
Patel et al. 2017) and recent neuroimaging studies in healthy adults show that
THC modulates activity in the amygdala and mPFC/rACC. Specifically, an acute
oral low dose of THC (7.5 mg) reduced amygdala reactivity, but enhanced coupling
between the amygdala and mPFC/rACC, to social threat (i.e., fearful and angry
facial expressions), as compared to placebo (PBO; Phan et al. 2008; Gorka et al.
2015a). These findings suggest that pharmacological enhancement of ECB signaling
may help to address corticolimbic dysfunction in PTSD and other stress-related
disorders. However, it should be noted that others have reported that
administration of THC, particularly at a higher dose (10 mg) increases amygdala
activation (Bhattacharyya et al. 2010, 2017), and modulates activation in
frontal and parietal regions (Crippa et al. 2009), while increasing levels of
anxiety and autonomic arousal to fearful faces (Crippa et al. 2009;
Bhattacharyya et al. 2010, 2017). These divergent findings highlight the
complexity of THC’s effect on threat responding that may be bimodal, such that
low doses of THC may be anxiolytic (Wachtel et al. 2002), whereas higher doses
of THC are typically anxiogenic (D’Souza et al. 2004; Genn et al. 2004; Viveros
et al. 2005b; Bhattacharyya et al. 2015, 2017). To-date, the effects of THC on
corticolimbic responses to threat have only been conducted in healthy
individuals. Thus, it is unclear whether the observed effects of THC on
corticolimbic function and functional connectivity would replicate in
individuals with trauma exposure who are at risk for developing PTSD and/or meet
criteria for PTSD."
and with reckless abandon as to how their findings
might be applied in law to the anti-happy brigade who profit from the miseries
of prohibition, they conclude:
"Consistent with previous findings in healthy adults,
we found that, within the PTSD group, THC attenuated amygdala activation,
increased mPFC/rACC activation, and increased corticolimbic functional
connectivity to threat compared to PBO (Phan et al. 2008; Gorka et al. 2015)."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7244361/ [1507]
In "The Long-Term, Prospective, Therapeutic Impact of
Cannabis on Post-Traumatic Stress Disorder" by Bonn-Miller et al (2022) decided:
"Given the increasing availability and use of cannabis
among individuals with post-traumatic stress disorder (PTSD) and the addition of
PTSD as an eligible diagnosis in several U.S. medical cannabis programs [24
states as of 2020], the efficacy of dispensary-obtained cannabis needs to be
thoroughly examined."
and to the extent that they were able to do so...
"This prospective study [see 2362 page 332 for
definition] assessed PTSD symptoms and functioning every 3 months over the
course of a year in two samples of participants diagnosed with PTSD: (1) those
with PTSD using dispensary-obtained cannabis (cannabis users) and (2) those with
PTSD, who do not use cannabis (controls). Linear mixed-effects models and
generalized estimating equations tested whether trajectories of symptoms
differed between the two subsamples."
And so
"A total of 150 participants (mean [standard
deviation] age, 50.67 [15.26] years; 73% male) were enrolled in the study. Over
the course of 1 year, the cannabis users reported a greater decrease in PTSD
symptom severity over time compared to controls [group×time interaction=−0.32
(95% confidence interval [CI]=−0.59 to −0.05, R2=0.13; t=−2.35, p=0.02).
Participants who used cannabis were 2.57 times more likely to no longer meet
DSM-5 criteria for PTSD at the end of the study observation period compared to
participants who did not use cannabis (95% CI=1.12–6.07; p=0.03)."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9070744/ [1509]
In "Anxiety severity and prescription medication
utilization in first-time marijuana users" from Dugosh et al (2023):
"The study sample was comprised of 108 adults with
anxiety or PTSD as a referring condition; they were enrolled in a longitudinal
study evaluating biopsychosocial outcomes in new MM patients. Consenting
participants completed an assessment battery at baseline and Month 3 (n = 94, 87
% follow-up rate) that included a measure of anxiety severity and questions
about current anxiety medication prescription and desired (baseline) and actual
(Month 3) reductions in medication use.
"Results
Findings indicated that 59 % of participants reported
prescription medications for anxiety, with 70 % reporting at least a moderate
desire to reduce medication use. Overall and within the medication sub-sample,
participants displayed significant reductions in anxiety severity from baseline
to Month 3 (p’s <0.0001). Furthermore, 32 % reported actual reductions in
medication use at Month 3, and reductions were more likely among patients
prescribed benzodiazepines than other drug classes.
"Conclusions
Results suggest that a significant number of MM
patients with anxiety and/or PTSD diagnoses are currently being prescribed
antianxiety medications and that MM may help to reduce their use of these
medications.
"Limitations
Limitations include the observational study design and
the lack of a PTSD-specific measure. More controlled longitudinal studies are
necessary to better understand the role of MM in the treatment of anxiety and
PTSD."
https://www.cannabisclinicians.org/2023/10/27/anxiety-severity-and-prescription-medication-utilization-in-first-time-medical-marijuana-users-2/
[4190]
Again, in 2023, Vaddiparti et al found
"PTSD symptom severity as measured by total PCL-5
score improved significantly at 30- and 70-day follow-ups. Similarly,
statistically significant reductions in nightmares were reported at 30- and
70-day follow-ups. Corresponding improvements in sleep were noticed with
participants reporting increased duration of sleep hours, sleep quality, sleep
efficiency, and total PSQI score. Likewise, negative affect and global mental
health improved significantly at follow-up. According to the post hoc analyses,
the most statistically significant changes occurred between baseline and 30-day
follow-up. The exception to this pattern was nightmares, which did not show
significant improvement until day 70."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10642978/ [4254]
In 162 patients with PTSD identified from the UK
Medical Cannabis Registry, tested with Impact of Events Scale-Revised (IES-R),
EQ-5D-5L, Single-Item Sleep Quality Scale (SQS), Generalized Anxiety Disorder-7
(GAD-7) and Patient Global Impression of Change (PGIC), Pillai et al (2022)
found that:
"Statistically significant improvements were seen in
all domains of the IES-R, and both GAD7 and SQS, at all lengths of follow-up (p
< 0.050). The EQ-5D-5L index score and both ‘usual activities’ and ‘anxiety
and/or depression’ subscales also improved significantly at all follow-ups (p <
0.050). Significant improvements in the ‘self-care’ and ‘pain and discomfort’
subscales were seen at 1- and 3-month follow-up and the ‘mobility’ subscale at
3-months only (p < 0.050). There was a large effect size (r = 0.50) for the
IES-R hyperarousal score at 3-month follow-up. All other IES-R and GAD7 scores
had medium effect sizes. PGIC1 median scores were consistently 6.00 (5.00–6.00)
at 1-, 3-, and 6-month follow-up, whilst median PGIC2 was 3.00 (2.00–3.00) at 1-
and 3-month follow-up, and 2 (1.00–3.00) at 6-months (n = 128, 93, and 51
respectively)."
https://www.tandfonline.com/doi/full/10.1080/14737175.2022.2155139
[4694]
Mayo et al, reviewing the issue of "Targeting the
Endocannabinoid System in the Treatment of Posttraumatic Stress Disorder: A
Promising Case of Preclinical-Clinical Translation?" in 2022, say:
"Preclinical research shows that eCB activity
influences functional connectivity between the prefrontal cortex and amygdala
and thereby influences an organism’s ability to cope with threats and stressful
experiences. Animal studies show that CB1 receptor activation within the
amygdala is essential for extinction of fear memories. Failure to extinguish
traumatic memories is a core symptom of posttraumatic stress disorder,
suggesting that potentiating eCB signaling may have a therapeutic potential in
this condition. However, it has been unknown whether animal findings in this
domain translate to humans. Data to inform this critical question are now
emerging and are the focus of this review."
Under the headling "Fear" they say
"The loss-of-function FAAH 385A allele was inserted
into mice, resulting in decreased FAAH activity and concomitantly increased AEA
levels. In mice and humans, carriers of the A-allele had enhanced
fronto-amygdala connectivity and fear extinction. We subsequently reported
similar effects in humans, including a gene dose–dependent effect of the
A-allele on peripheral AEA levels. Individuals homozygous for the A-allele
showed enhanced fear extinction and recall of extinction learning when tested 24
hours later. These findings have since been replicated by others, showing that
fear extinction is related to peripheral AEA levels."
And the latest scientists to discover cannabis think...
"The available human data consistently support a
translation of animal findings on fear memories and stress reactivity and
suggest a potential therapeutic utility in humans."
Their Figure 1 shows the approaches to ECS pathways
from a drug manufacturing perspective
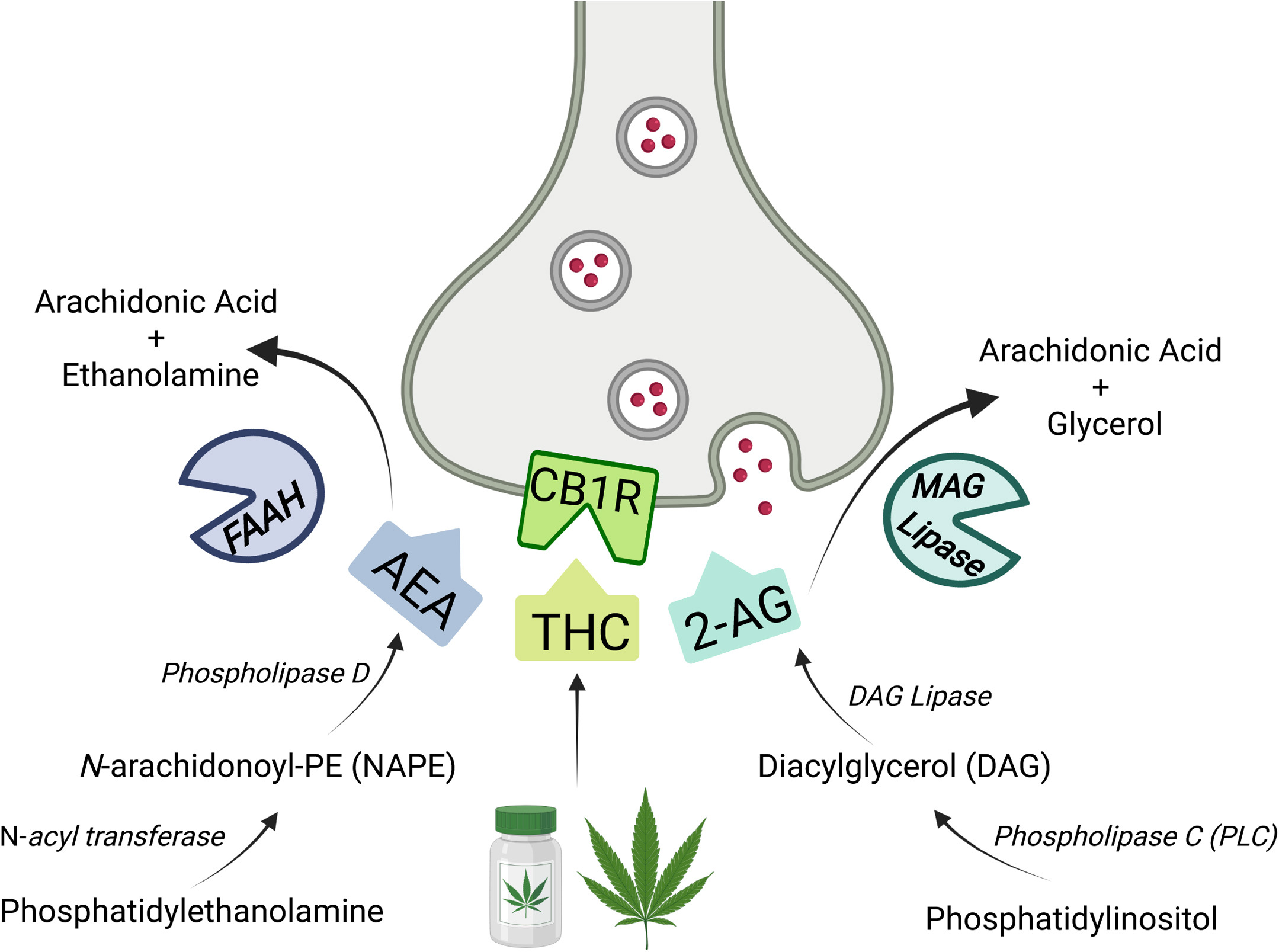
https://www.sciencedirect.com/science/article/pii/S0006322321014724
[4010]
Taking another overview of the evidence in 2023,
Marchetta et al
"...describe the three fear memory phases (e.g.,
consolidation, reconsolidation and extinction) that are most significantly
altered in PTSD patients, and...review data from both human and animal studies
on the effects of repeated exposure to trauma reminders on fear memory retention
and extinction combined with pharmacological intervention."
Highlights include
"Based on preclinical studies, the monoamine
hypothesis of PTSD has been enlarged with a more complex neurochemical and
neuroplasticity hypothesis that highlights the role of the glutamatergic system
in trauma and stress psychopathology."
"The mechanisms sustaining systems consolidation have
not been fully elucidated."
As for reconsolidation
"...differently to what the name might suggest, it is
not a simple replication of the consolidation phase, although overlaps between
the underlying mechanisms of these two phases exist. Studies in rodents have
demonstrated that memory may be disrupted via inhibition of new gene expression
or protein synthesis in the hippocampus immediately after retrieval of a
consolidated memory, whereas the same manipulations into the hippocampus long
after retrieval had no effect on memory. This indicates that these manipulations
are effective only when given soon after reactivation but not when given after a
delay. In addition, consolidated memories that are not retrieved, and therefore
do not become labile, cannot be disrupted by the inhibition of gene expression
or protein synthesis. Hence, if a consolidated memory could turn back to its
labile state and be disrupted by external interventions, some authors argue that
there might be the chance that the disruption of the original traumatic memories
could be an efficacious approach to treat PTSD patients."
Memory extinction was first commented upon by Pavlov
in 1927. Today...
"Extinction training is not the same as forgetting,
but it is considered as new learning because it leaves the CS as having two
meanings: 'fear' if coupled with the US or 'safe' if it is not coupled with US.
When memory is extinguished, it means that the 'safe' prevails over the 'fear'
meaning. Many studies have provided evidence demonstrating that extinction
consists of a new learning process. Specifically, without extinction training,
the fear response lasts months or even years, and extinguished fear responses
return naturally with the passage of time (spontaneous recovery), after using a
different context compared with the one in which extinction training took place
(renewal), or as a consequence of the re-exposure to the US (reinstatement)"
%202490.jpg)
The authors'
"Literature search was conducted in March, 2021 by
comprehensive searches in two online databases (PubMed and Scopus). The keywords
used for the search of animal studies were: D-cycloserine, yohimbine, methylene
blue, glucocorticoids or corticosterone or methyrapone, cannabinoids or
endocannabinoids, MDMA or 3-4, methylenedioxymethamphetamine, ketamine,
psychedelics and/in post traumatic stress disorder or posttraumatic stress
disorder or posttraumatic stress disorder or fear memory or memory extinction or
memory reconsolidation. Results were limited to rodents studies. The keywords
used for the search of human studies were: D-cycloserine, yohimbine, methylene
blue, glucocorticoids or cortisol, cannabinoids or endocannabinoids, MDMA or
3-4, methylenedioxymethamphetamine, ketamine, psychedelics and/in post traumatic
stress disorder or posttraumatic stress disorder or post-traumatic stress
disorder. For both the 1st (i.e., titles and abstracts) and the 2nd (i.e.,
full-text articles) screening phases, the following exclusion criteria were
used: (1) papers written in a language other than English; (2) non-original
researches (e.g., reviews, commentaries, editorials, book chapters); (3) no
full-text articles (e.g., meeting abstracts); (4) studies in vitro; (5) studies
in non-human animals other than rodents; (6) drugs administration not associated
with an animal model of PTSD or psychological intervention in humans; (7)
absence of control groups in the studies."
As for cannabinoids:
"The eCBs AEA and 2-AG are mainly degraded by two
enzymes fatty-acid amide hydrolase (FAAH) and monoacylglycerol lipase (MAGL),
respectively. Increasing number of animal studies suggests that eCB signaling is
critically involved in the extinction phase of fear memory. Several reports have
demonstrated that increased AEA signaling, through inhibition of FAAH activity,
induced an enhancement of fear memory extinction. On the contrary, the
administration of CB1 receptor antagonists impaired the extinction and
reconsolidation of fear memory. In accordance with these results, CB1 KO mice or
mice bearing the FAAH C385A polymorphism, which impairs the activity of FAAH,
showed reduced and enhanced fear memory extinction, respectively, thus,
supporting the hypothesis that strengthening AEA signaling at CB1 receptors
enhances fear extinction. In a PTSD-like rat model, we have recently
demonstrated that the FAAH inhibitor URB597 or the direct cannabinoid receptor
agonist WIN55,212-2 (Fig. 1) enhanced fear extinction tested 16 days
post-trauma, when administered after three spaced extinction sessions, 7, 10 and
13 days after trauma exposure. Both drugs showed beneficial effects, but only
URB597 (0.1 mg/kg, i.p.) induced the best improvements by enhancing extinction
consolidation and restoring normal social behavior in traumatized rats through
indirect activation of CB1 receptors tested up to 36-37 days post-trauma.
Further, another recent study has confirmed these findings in male rodents
showing beneficial effects on fear extinction of the FAAH inhibitor URB597.
Contrarily to what has been found and described above in males, increased AEA
signaling at CB1 receptors (Fig. 1), 60 min prior to extinction training in an
auditory fear conditioning paradigm, did not alter fear memory extinction in
female rats. However, when AEA signaling was increased at the transient
potential receptor of vanilloid type-1 channel (TRPV1R, another target of AEA
beyond CB1 receptors), it augmented freezing behavior at extinction training and
extinction retrieval. Increased 2- AG signaling at CB1 receptors reduced
freezing at extinction training in females, without altering fear responses in
males."
But in humans, they believe:
"Rigorous clinical studies regarding the efficacy of
cannabinoids for PTSD in conjunction with psychotherapy are still lacking."
As for psychedelics Marchetta et al say:
"Psylocibin, lysergic acid diethylamide (LSD) and
dimethyltryptamine share a common mechanism of agonism at serotonergic 5-HT2A
receptor. Although few studies have indicated possible use of these psychedelics
for depression and obsessive-compulsive disorder, no other study has yet been
reported regarding a potential treatment for PTSD. However, the effects on
empathy, mindfulness related capacities, avoidance, acceptance and
connectedness, long-term openness, and emotional break-through experiences along
with preclinical studies, demonstrating an enhancing effect on fear memory
extinction, should determine a renewed interest on these compounds."
https://pmc.ncbi.nlm.nih.gov/articles/PMC10207915/
[2490]
But were those clinical
studies really "still lacking" in 2023?
The Prosecution should have been fully aware, by the early 2000s, of the
implications of taking away phytocannabinoids it said had no medical utility:
"Seminal research in the early 2000s revealed that, in vitro, the
glucocorticoid-based inhibition of paraventricular nucleus neurons and the
subsequent inhibition of corticotropin-releasing hormone synthesis depended on
retrograde endocannabinoid signalling. Research in the early 2000s also found
that corticotropin-releasing hormone was found to be highly co-expressed with
CB1 receptors in the forebrain. It was, therefore, suspected that
endocannabinoids could be involved in the regulation of the
hypothalamic–pituitary–adrenal (HPA) axis response to stress. Subsequent
research confirmed this hypothesis, as it was discovered that a reduction in AEA
in the basolateral amygdala is required for HPA axis activation, suggesting that
AEA tonically gates the HPA response. Research further explored the mechanisms
involved in HPA gating by AEA and found that CRH-mediated increases in FAAH
expression is responsible for the decrease in amygdala AEA prior to HPA onset.
"While AEA is believed to tonically gate the HPA stress response, 2-AG is
believed to be involved in the termination of the response through the
facilitation of glucocorticoid-mediated negative feedback. Research that
supports this hypothesis has shown that 2-AG levels increase in the hippocampus
30 to 60 min following stress, while the inhibition of CB1 in the frontal areas
of the brain prevents negative feedback of the HPA axis. Likewise, the
inhibition of MAGL, but not FAAH, maintains increased corticosterone expression
after stress onset. Given the evidence described above, it has therefore been
widely hypothesised that endocannabinoids are involved in both the initiation
and termination of the HPA axis response to stress." [5126]
The Court is invited to evaluate the validity of the
statement that "no other study has yet been reported regarding a potential
treatment for PTSD" [2490]
with psychedelics. No one has scientifically proved that I will cheer up if I
have a cup of tea. But that doesn't mean that I won't.
Then, in September 2023, Cell Reports published a
study. Here are some key facts, as reported by neurosciencenews.com:
"Summary: A recent study illuminates the brain’s
unique response to stress: releasing its own cannabinoid molecules akin to THC
from cannabis plants.
"Centered in the amygdala, these molecules counteract
stress alarms originating from the hippocampus, an integral memory and emotion
region. This hints at the body’s intrinsic mechanism for stress management.
"Disruption in this system might escalate risks for
stress-induced psychiatric conditions.
"Key Facts:
"The amygdala, an emotional brain center, releases
endogenous cannabinoids to mitigate stress, interacting with the same receptors
as THC.
"When the target cannabinoid receptor was removed in
mice, there was a noticeable decline in their ability to handle stress and a
diminished inclination towards rewarding experiences.
"This study further supports the endocannabinoid
system’s role as a potential drug-development candidate for stress-related
disorders."
https://neurosciencenews.com/endocannabinoids-stress-23913/ [3011]
According to the paper:
"BLA activity promotes eCB release at vHPC-BLA
synapses
"Active stress coping recruits vHPC-BLA eCB signaling
"vHPC-BLA CB1 receptor deletion exacerbates
stress-induced avoidance/anhedonia
"The endocannabinoid (eCB) system is a key modulator
of glutamate release within limbic neurocircuitry and thus heavily modulates
stress responsivity and adaptation. The ventral hippocampus (vHPC)-basolateral
amygdala (BLA) circuit has been implicated in the expression of negative
affective states following stress exposure and is modulated by retrograde eCB
signaling. However, the mechanisms governing eCB release and the causal
relationship between vHPC-BLA eCB signaling and stress-induced behavioral
adaptations are not known. Here, we utilized in vivo optogenetic- and
biosensor-based approaches to determine the temporal dynamics of
activity-dependent and stress-induced eCB release at vHPC-BLA synapses.
Furthermore, we demonstrate that genetic deletion of cannabinoid type-1
receptors selectively at vHPC-BLA synapses decreases active stress coping and
exacerbates stress-induced avoidance and anhedonia phenotypes. These data
establish the in vivo determinants of eCB release at limbic synapses and
demonstrate that eCB signaling within vHPC-BLA circuitry serves to counteract
adverse behavioral consequences of stress."
Vanderbilt University, Tennessee, authors Kondev et al
(2023) say where this gets us to:
"A key question arises from our previous data
demonstrating relatively enhanced DSE at vHPC-BLA synapses in stress-resilient
mice and from our current data revealing 2-AG release at vHPC-BLA synapses in
response to stress exposure: is 2-AG-CB1R signaling at vHPC-BLA synapses
causally linked to stress-induced behavioral reactivity and adaptation? Our data
address this question in two separate, but related, ways. First, we found that
2-AG release occurred during bouts of active stress coping that were preceded by
increases in BLA neuron activity. Combined with previous data suggesting that
BLA activity (or activity of a subset of BLA output neurons) is associated with
active behavioral responses to stress, this suggests a possible scenario whereby
increases in BLA activity drive 2-AG release to dampen vHPC afferent excitation
via activation of presynaptic CB1R. That deletion of CB1R from vHPC-BLA
terminals reduced active stress coping in a variety of assays (restraint stress,
TST, FST) suggests that vHPC inputs to the BLA promote passive stress coping.
This hypothesis is consistent with data demonstrating that vHPC-BLA circuits are
critical for driving freezing responses to contextual threat. How vHPC inputs to
the BLA selectively drive 'passive' output circuits or inhibit 'active' output
circuits from the BLA is not known but represents an important open question.
Second, we found that deletion of CB1R from vHPC-BLA synapses promotes anhedonia
and avoidance selectively after stress exposure and, more robustly, after
repeated stress exposure. These data suggest that 2-AG released within the
synapse during stress exposure plays an important role in buffering against
subsequent adverse behavioral consequences of stress, consistent with previous
studies. Taken together, these data indicate that 2-AG-CB1 signaling at vHPC-BLA
synapses plays an important role in regulating behavioral responses during and
after stress exposure and provides further support for the contention that 2-AG
signaling within defined limbic circuits is a critical mechanism buffering
against the adverse effects of stress exposure. A key question arises from our
previous data demonstrating relatively enhanced DSE at vHPC-BLA synapses in
stress-resilient mice and from our current data revealing 2-AG release at
vHPC-BLA synapses in response to stress exposure: is 2-AG-CB1R signaling at
vHPC-BLA synapses causally linked to stress-induced behavioral reactivity and
adaptation? Our data address this question in two separate, but related, ways.
First, we found that 2-AG release occurred during bouts of active stress coping
that were preceded by increases in BLA neuron activity. Combined with previous
data suggesting that BLA activity (or activity of a subset of BLA output
neurons) is associated with active behavioral responses to stress, this suggests
a possible scenario whereby increases in BLA activity drive 2-AG release to
dampen vHPC afferent excitation via activation of presynaptic CB1R. That
deletion of CB1R from vHPC-BLA terminals reduced active stress coping in a
variety of assays (restraint stress, TST, FST) suggests that vHPC inputs to the
BLA promote passive stress coping. This hypothesis is consistent with data
demonstrating that vHPC-BLA circuits are critical for driving freezing responses
to contextual threat. How vHPC inputs to the BLA selectively drive 'passive'
output circuits or inhibit 'active' output circuits from the BLA is not known
but represents an important open question. Second, we found that deletion of
CB1R from vHPC-BLA synapses promotes anhedonia and avoidance selectively after
stress exposure and, more robustly, after repeated stress exposure. These data
suggest that 2-AG released within the synapse during stress exposure plays an
important role in buffering against subsequent adverse behavioral consequences
of stress, consistent with previous studies.
"Taken together, these data indicate that 2-AG-CB1
signaling at vHPC-BLA synapses plays an important role in regulating behavioral
responses during and after stress exposure and provides further support for the
contention that 2-AG signaling within defined limbic circuits is a critical
mechanism buffering against the adverse effects of stress exposure."
https://www.cell.com/cell-reports/fulltext/S2211-1247(23)01038-0 [3012]
In their 2022 paper "Neuroinflammation in
Post-Traumatic Stress Disorder" Dong-Hun Lee and colleagues at the Department of
Neurosurgery, College of Medicine, Soonchunhyang University, Cheonan Hospital,
Korea, pointed to pro-inflammatory cytokines as biomarkers of PTSD:
"The Marine Resiliency Study reported that preexisting
concentrations of C-reactive protein (CRP) were directly correlated with the
occurrence and severity of PTSD, three months after a seven-month military
deployment, and elevated levels of interleukin (IL)-6, IL-8, and transforming
growth factor β (TGF-β) during hospitalization predicted the development of PTSD
one month later. These data suggest that immune dysregulation predisposes
individuals to PTSD. The elevation of inflammatory cytokines in PTSD has
clinical significance, as chronic inflammation can adversely affect
cardiovascular and physical health. In addition, individuals with PTSD are
significantly more likely to suffer autoimmune disorders compared with those
with other psychiatric conditions. Inflammation-related mediators, such as IL-1,
IL-6, and tumor necrosis factor alpha (TNF-α), may pass through the blood–brain
barrier, and the overproduction of pro-inflammatory cytokines can activate brain
microglia. A few small studies have examined the cerebrospinal fluid levels of
cytokines in PTSD but have yielded conflicting results."
We like the large studies.
"One of the largest studies exclusively of men exposed
to combat trauma reported a significantly elevated pro-inflammatory composite,
comprising IL-1β, IL-6, TNF-α, IFN-γ, and CRP levels in those with PTSD compared
to those without PTSD. The predominant cytokines were different for each group,
and differences were observed in TNF-α, IFN-γ, and IL-6 values. The
pro-inflammatory cytokine levels remained significantly higher in individuals
with PTSD after controlling for early-life trauma, major depressive disorder and
its severity, body mass index, ethnicity, education, asthma and/or allergies,
time since combat, potentially confounding inflammatory illnesses, and
medications. Immune activation of PTSD was also found to be significantly high
in male groups who experienced combat trauma.
"Conversely, several other studies have reported no
significant difference in inflammatory marker levels between patients with PTSD
and healthy controls."
Lee et al discuss the role of DAMP, HPA axis,
serotonin and tryptophan–kynurenine pathways:
"Damage-associated molecular patterns (DAMPs) are
host-derived non-bacterial immune response molecules released due to
PTSD-related stress. These molecules act as danger signals when cells are
damaged. When DAMPs are released from cells, pattern recognition receptors
(PRRs) are expressed in astrocytes and microglia to promote neuroinflammatory
reactions. The PRR is a protein expressed by innate immune system cells such as
dendritic cells, macrophages, monocytes, and neutrophils, and is a receptor that
recognizes DAMPs and plays an important role in innate immunity. One of the
PRRs, the Toll-like receptor (TLR), is expressed in various cells of the CNS,
including neurons, microglia, and astrocytes. These PRRs are activated by
detecting endogenous molecules such as DAMPs, and the persistent
neuroinflammatory action of glial cells can lead to neurodegeneration."
and
"IL-1 receptors (IL-1Rs) are produced by microglia,
astrocytes, and brain oligodendrocytes, and have been shown to be highly
concentrated in the pituitary and meninges. IL-1R mRNA is expressed in the
capillaries and glial cells throughout the hippocampus, choroid plexus,
cerebellum, and brain, and the IL-1 type 1 receptor is expressed in humans’
hypothalamus. The secreted inflammatory cytokines are received in these glial
cells and contribute to neuroinflammation. Therefore, the impairment of the HPA
axis due to PTSD can lead to neuroinflammation."
and
"Tryptophan is an essential amino acid used in protein
biosynthesis and is mainly metabolized with kynurenine. Kynurenine is a
metabolite of tryptophan that performs a variety of biological functions,
including vasodilation and immune response during inflammation. This kynurenine
pathway is modified in several diseases, including mental disorders such as
schizophrenia and depressive disorders. Pro-inflammatory cytokines can enhance
the activity of indolamine 2,3-dioxigenase (IDO), the first and rate-limiting
enzyme in the tryptophan degradation pathway. Elevated levels of
pro-inflammatory cytokines increase IDO enzyme activity. IDO is involved in
tryptophan metabolism, which upregulates the production of kynurenine.
Kynurenine is converted into several metabolites, including quinolinic and
kynurenic acids, and it is involved in the activity and inhibition of NMDA
(N-methyl-d-aspartate), with elevated pro-inflammatory cytokines producing
relatively larger amounts of quinolinic acid (Figure 4). This increase in
quinoline acid has a potent neurotoxic effect, which can activate microglia and
macrophages, increase reactive oxygen and reactive nitrogen species due to lipid
peroxidation, and interfere with nerve function or cause apoptosis. Some studies
have also shown that quinoline acid may also be linked to mental disorders,
although the mechanism is still unclear. However, quinoline acid has been found
in the postmortem brain of depressed patients."
The authors briefly mention cannabis, and claim rather
ignorantly
"...very few studies have reported the potential
usefulness of cannabis in the treatment of PTSD."
In Korea, perhaps. There are only 13.9 million Google
results for "cannabis ptsd korea". However these authors suggest a variety of
drug treatments including NSAIDs, steroids, angiotensin-converting enzyme
inhibitors and angiotensin receptor blockers, and invasive treatments like deep
brain stimulation (DBS).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9138406/ [4076]
In 2007 Miller and Wrosch found that carrying on with
unattainable goals appears to affect C-reactive protein.
"The notion that persistence is essential for success
and happiness is deeply embedded in popular and scientific writings. However,
when people are faced with situations in which they cannot realize a key life
goal, the most adaptive response for mental and physical health may be to
disengage from that goal. This project followed 90 adolescents over the course
of 1 year. Capacities for managing unattainable goals were assessed at baseline,
and concentrations of the inflammatory molecule C-reactive protein (CRP) were
quantified at that time, as well as 6 and 12 months later. To the extent that
subjects had difficulties disengaging from unattainable goals, they displayed
increasing concentrations of CRP over the follow-up. This association was
independent of potential confounds, including adiposity, smoking, and
depression. Because excessive inflammation contributes to a variety of adverse
medical outcomes, these findings suggest that in some contexts, persistence may
actually undermine well-being and good health."
https://pubmed.ncbi.nlm.nih.gov/17760771/ [4698]
We underestimate the effect of trauma on third
parties, as shown by Song et al in "Firearm Injuries In Children And
Adolescents: Health And Economic Consequences Among Survivors And Family
Members" (2023):
"More US children and adolescents today die from
firearms than any other cause, and many more sustain firearm injuries and
survive. The clinical and economic impact of these firearm injuries on survivors
and family members remains poorly understood. Using 2007–21 commercial health
insurance claims data, we studied 2,052 child and adolescent survivors compared
to 9,983 matched controls who did not incur firearm injuries, along with 6,209
family members of survivors compared to 29,877 matched controls, and 265 family
members of decedents compared to 1,263 matched controls. Through one year after
firearm injury, child and adolescent survivors experienced a 117 percent
increase in pain disorders, a 68 percent increase in psychiatric disorders, and
a 144 percent increase in substance use disorders relative to the controls.
Survivors’ health care spending increased by an average of $34,884—a 17.1-fold
increase—with 95 percent paid by insurers or employers. Parents of survivors
experienced a 30–31 percent increase in psychiatric disorders, with 75 percent
more mental health visits by mothers, and 5–14 percent reductions in mothers’
and siblings’ routine medical care. Family members of decedents experienced
substantially larger 2.3- to 5.3-fold increases in psychiatric disorders, with
at least 15.3-fold more mental health visits among parents. Firearm injuries in
youth have notable health implications for the whole family, along with large
effects on societal spending."
https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2023.00587 [4085]
Clearly, individuals vary in their susceptibility to PTSD for a variety of
reasons. Unusual long-term background stressors and acute trauma have conspired
against the Defendant's well-being fully justifying continued use of both
cannabis and psychedelics with no need for therapy. Indeed in one unpopular
paper it was shown that therapists add no value to psychedelics: "no significant
association was found between the number of therapy hours and outcome in either
the short-term (b = −0.05, p = .327) or long-term."
https://www.sciencedirect.com/science/article/pii/S0163834325001562 [5294]
In the view of the Defendant and most illicit users, therapy is a two-edged
sword, as likely to undermine the confidence of the subject as rebuild it.
Exploitation is a real probability, best averted not by having no unsupervised
psychedelicism, but by having no therapist.
Psychiatrists reinforce the sick role.
150 years ago the concept did not really exist.
Psychedelic therapy could make someone else legally and morally liable for a
person's mistakes.
Therapists are more expensive than real friends.
Therapists may try to do too many things at once, not all of them for the
"patient".
As in the wider field of psychiatry, psychedelic therapy is an attempt at
labelling all users as mentally ill in one way or another.
And with those endless categories and theories, and mental confusion about
"drugs", even with mushrooms welcomed back into the pharmaceutical fold,
psychiatrists can start out meaning well...but they face difficulties being part
of the set and setting of a therapeutic journey, with psychedelics or without.
9 to 40 million years after the first biosynthesis of psilocybin [3252]
individual vulnerability to PTSD was addressed by Suprani et al [2025]:
"While the symptom burden can be substantial-particularly in high-risk
populations exposed to cumulative or prolonged trauma-the lifetime prevalence of
full-syndrome PTSD in the general population remains lower; for instance, it is
estimated at 6.1% in the United States. Epidemiological evidence has
consistently shown that only a minority of trauma exposed individuals go on to
develop PTSD. The neurobiological mechanisms underpinning the individual
variation in vulnerability to PTSD development following trauma are still
unclear. Different biological systems have been investigated, such as those
involved in neuroplasticity and immunoregulation. More recently, the
endocannabinoid (eCB) system has received attention in the PTSD research field,
given its modulatory effect on memory consolidation, retrieval and extinction.
There is a large amount of data in animal models supporting the eCB system role
in regulating fear and stress responses. The fatty acid-derived signaling
molecule Anandamide (AEA), the first discovered endocannabinoid, was shown to
facilitate fear extinction in mice by activating the Cannabinoid receptor 1
[CB1]. When research on the eCB system in fear responses was extended to humans,
consistent results were found, mostly on healthy subjects. Three different human
studies replicated the association between enhanced fear extinction and a
hypofunctional genetic variation in the fatty acid amide hydrolase (FAAH), an
enzyme that catabolizes AEA. Positive results in genetics research were also
published by Heitland et al., who found that A/A carriers of rs2180619 (a
polymorphism located in the promoter region of CB1), exhibited impaired fear
extinction. In line with preclinical and healthy volunteers’ literature,
individuals with PTSD were shown to have a reduction in circulating
endocannabinoids levels.
"A recent study identified the amygdala-projecting medial prefrontal cortex
(mPFC) neurons as a potential neural basis for the effect of the eCB system on
fear extinction. The amygdala is a primary hub in the brain that regulates the
processing of aversive memories, by integrating information from different
cortical brain regions. Among these regions, the mPFC was shown to exert
top-down control of negative emotions over the amygdala in mice. Findings in
patients with PTSD suggest that the interaction between the mPFC and the
amygdala becomes dysfunctional, resulting in the heightened responsivity of the
latter. Several recent studies with different designs support this hypothesis.
For instance, neurosurgical patients with ventral mPFC lesions exhibited
potentiated amygdala responses to aversive images compared to neurologically
healthy controls. Consistently, Feng et al., showed that the resting-state
functional connectivity between the ventral mPFC and the amygdala is positively
correlated with fear extinction after fear reminder in healthy subjects.
Overall, numerous lines of evidence point toward a potential role of the eCB
system in PTSD vulnerability following trauma, possibly via altered top-down
control on the amygdala."
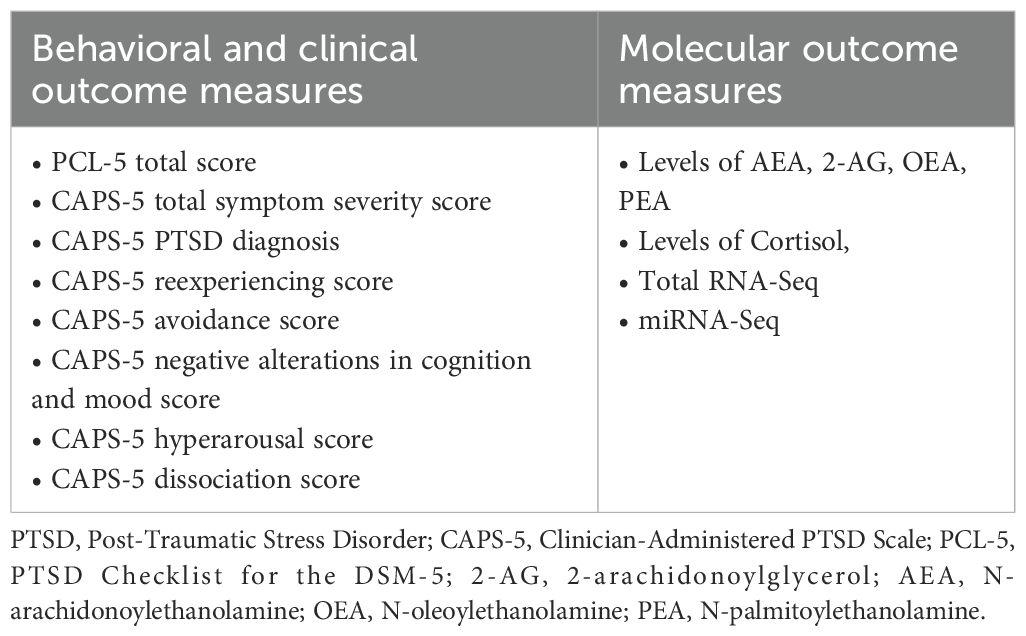
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1584583/full
[5295]
In "The Effectiveness and Adverse
Events of Cannabidiol and Tetrahydrocannabinol Used in the Treatment of Anxiety
Disorders in a PTSD Subpopulation" (2023) from Stack et al of the University of
Sydney's School of Pharmacology and Applied Cannabis Research in Sydney, NSW,
Australia:
"The median doses taken were 50.0
mg/day for CBD and 4.4 mg/day for THC. The total participant sample reported
significantly improved anxiety, depression, fatigue, and ability to take part in
social roles and activities. Those who were diagnosed with PTSD (n = 57)
reported significantly improved anxiety, depression, fatigue, and social
abilities. The most common AEs reported across the whole participant cohort were
dry mouth (32.6%), somnolence (31.3%), and fatigue (18.5%), but incidence varied
with different cannabis formulations. The inclusion of THC in a formulation was
significantly associated with experiencing gastrointestinal AEs; specifically
dry mouth and nausea. Conclusions: Formulations of cannabis significantly
improved anxiety, depression, fatigue, and the ability to participate in social
activities in participants with anxiety disorders. The AEs experienced by
participants are consistent with those in other studies."
And of special note:
"Participants who took a THC-dominant
formulation reported a significant decrease in their anxiety levels. Those same
participants also represented the highest proportion of participants that were
classified as having clinical improvement (61.1%, n = 11), compared with
participants who were prescribed other formulation types. This was unexpected as
the median THC dose for this participant group was 33.8 mg/day, and it has been
suggested that doses higher than 30 mg/day could be anxiogenic.14 A study
reported that doses of CBD ranging from 15 to 60 mg/day could offset the
anxiogenic properties of THC, which is reflected in our data; however, with
lower doses of CBD (median = 6.0 mg/day CBD)."
https://journals.sagepub.com/doi/pdf/10.1177/87551225231180796 [4557]
epidemic declared March 12 then again
October 19 2020
102 C/C polymorphism and suicide
Several lines of evidence indicate
that abnormalities in the functioning of the central serotonergic system are
involved in the pathogenesis of depressive illness and suicidal behavior.
https://pubmed.ncbi.nlm.nih.gov/19224112/ [298]
https://pubmed.ncbi.nlm.nih.gov/29526601/ [299]
https://pubmed.ncbi.nlm.nih.gov/11727894/ [300]
Research does not seek to eliminate
environmental influences in favour of genetic disposition in depression,
suicidal ideation and completed suicide. But there are only two hypotheses for
the high incidence in Slovenia, both of which may be right, namely that some are
genetically predisposed to snap when stress is prolonged or reaches a certain
level, or that living conditions for some, according to the rules constructed by
their own society, are relentlessly sub-optimal.
Slovenia is an ideal candidate for
psychedelic therapy. Slovenia ruminates endlessly about the past. Millions of
tonnes of CO2 are expended generating hot air about long-dead regimes and
ideologies, because they have affected people in this area. But arguing about
what Tito wrote about Stalin in 1940 won't bring your dead relatives back or
make you happy and strong today. To ignore the past and bury the hatchet seems
like a cop-out. But the past is getting in the way of the present, and the
future.
"In 1976, a man known as Ka-Tzetnik
135633 (original name: Yehiel De-Nur) underwent LSD-assisted psychotherapy. At
the time, he was under the supervision of Prof. Jan Bastiaans at the State
University of Leiden in the Netherlands. Bastiaans was the psychiatrist who had
first identified concentration camp syndrome, also known as survivor syndrome.
This syndrome is a form of what we would now call post-traumatic stress disorder
(PTSD). Its characteristics include social withdrawal, sleep disturbance,
anxiety, and depression. Bastiaans had also successfully treated this syndrome
with LSD-assisted psychotherapy. Ka-Tzetnik 135633 was a survivor of Auschwitz,
where he was a prisoner for two years. This trauma was followed by three decades
of torment, in which he relived the horror of those two years at night. Through
LSD-assisted psychotherapy, however, Ka-Tzetnik 135633 found healing.
"Almost a half century after
Bastiaans' successful trials, the regulation of psychedelics for treating PTSD
is finally underway. Think of the Holocaust survivors who might have found
healing through these medicines, but couldn't because of a politically-motivated
ban on psychedelics. This realization brings home the horrific impact of the
failed war on drugs.'"
https://realitysandwich.com/psychedelics-and-judaism/ [1092]
Psychedelics break the rumination
cycle by disrupting - in a good way - brain activities which perpetuate habitual
thinking and behaviour.
The most abundant 5-HT receptors
expressed in the medial prefrontal cortex (mPFC) are 5-HT1AR and 5-HT2AR. The
5-HT2AR pathway is enhanced by 5-HT2AR-agonist psychedelics.
https://pubmed.ncbi.nlm.nih.gov/28858536/ [301]
In mice, given a single dose of
psilocybin or LSD, and using the social reward conditioned place preference
(sCPP) assay Nardou et al have made an important step forward in understanding
the mechanism by which psychedelics can override cultural log-jams retarding
progress and societal happiness, such as we see in Slovenia. "Psychedelics
reopen the social reward learning critical period" (2023) finds:
"Psychedelics are a broad class of
drugs defined by their ability to induce an altered state of consciousness.
These drugs have been used for millennia in both spiritual and medicinal
contexts, and a number of recent clinical successes have spurred a renewed
interest in developing psychedelic therapies. Nevertheless, a unifying mechanism
that can account for these shared phenomenological and therapeutic properties
remains unknown. Here we demonstrate in mice that the ability to reopen the
social reward learning critical period is a shared property across psychedelic
drugs. Notably, the time course of critical period reopening is proportional to
the duration of acute subjective effects reported in humans. Furthermore, the
ability to reinstate social reward learning in adulthood is paralleled by
metaplastic restoration of oxytocin-mediated long-term depression in the nucleus
accumbens. Finally, identification of differentially expressed genes in the
‘open state’ versus the ‘closed state’ provides evidence that reorganization of
the extracellular matrix is a common downstream mechanism underlying psychedelic
drug-mediated critical period reopening. Together these results have important
implications for the implementation of psychedelics in clinical practice, as
well as the design of novel compounds for the treatment of neuropsychiatric
disease."
https://www.nature.com/articles/s41586-023-06204-3 [2825]
But we do not need to rely on mice
when there are real-life mass traumas going on. A special opportunity came along
on 7 October 2023 in the Hamas attack on Supernova. "Trauma Under Psychedelics:
MDMA Shows Protective Effects During the Peritraumatic Period" say Netzer et al
(2024):
"Traumatic events (TEs) play a causal
role in the etiology of psychopathologies such as depression and posttraumatic
stress disorder (PTSD). Recent research has highlighted the therapeutic
potential of psychoactive substances and especially
3,4-methylenedioxymethamphetamine (MDMA), in alleviating trauma symptoms in
chronic patients. However, little is known regarding the consequences of trauma
that is acutely experienced under the influence of psychoactive substances. Here
we investigated the acute experiences and peritraumatic processing of 657
survivors from the high-casualty terror attack at the Supernova music festival
in Israel on October 7th, 2023. Data were collected four to twelve weeks
following the TE. Approximately two-thirds of survivors were under the influence
of psychoactive substances at the time of the TE, offering a tragic and unique
natural experiment on the impact of psychoactive compounds on TE processing. Our
findings reveal that individuals who experienced the trauma while under the
influence of MDMA demonstrated significantly improved intermediate outcomes
compared to those who were under the influence of other substances or no
substances at all. Specifically, the MDMA group reported increased feelings of
social support, more social interactions and enhanced quality of sleep during
the peritraumatic period, yielding reduced levels of mental distress and reduced
PTSD symptom severity. These novel findings suggest that the influence of MDMA
during the TE may carry protective effects into the peritraumatic period,
possibly mediated through the known effects of MDMA in reducing negative
emotions and elevating prosociality. These protective effects in turn may
mitigate the development of early psychopathology-related symptoms. Current
preliminary results underscore the need for further understanding of the
cognitive and physiological processes by which psychedelic substances intersect
with trauma recovery processes."
https://www.biorxiv.org/content/10.1101/2024.03.28.587237v1 [3174]
Another alternative to mice is "Human
pluripotent stem cells as a translational toolkit in psychedelic research in
vitro". As Salerno and Rehan explain:
"PSCs can differentiate into various
brain cell types, mirroring endogenous expression patterns and cell identities
to recreate disease phenotypes. Brain organoids derived from PSCs resemble cell
diversity and patterning, while region-specific organoids simulate circuit-level
phenotypes. PSC-based models hold significant promise to illuminate the cellular
and molecular substrates of psychedelic-induced phenotypic recovery in
neuropsychiatric disorders."
and
"The identities of the signaling
pathways responsible for psychedelics’ hallucinogenic and therapeutic properties
and whether these are distinct or overlapping pathways are some of the questions
still under debate.
"The Gq or β-arrestin-2 recruitment
paradigm represents a glimpse into the extensive network of pathways regulated
by 5-HT2AR activation via psychedelics. For example, distinct psychedelics
activate phospholipase A2 and phospholipase D via ADP-ribosylation factor 1. The
activation of 5-HT2AR, triggered by various agonists including DOI and LSD, can
lead to the heterodimerization of the receptor with metabotropic glutamate
receptor 2 and dopamine D2 receptor, both of which are Gi-coupled receptors.
This transactivation blocks the cAMP’s synthesis by adenylate cyclase and
prompts heterotrimeric Gi/o proteins to trigger Src-mediated downstream events.
"A burst of glutamate also follows
psychedelic administration, mainly in the cortical layer V of the neocortex,
which is a 5-HT2AR-enriched area.8,23 High glutamate levels activate the
α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR), boosting
the secretion of brain-derived neurotrophic factor (BDNF), which in turn signals
through the tyrosine receptor kinase B (TrkB) and mammalian target of rapamycin
(mTOR) pathways, sustaining both the AMPAR activation and BDNF secretion in a
positive feedback loop of neural plasticity.
"Furthermore, the hallucinogenic
properties of different psychedelics are also proposed to be influenced by other
5-HTRs, and not all 5-HT2AR agonists have hallucinogenic properties. For
instance, human studies also provide evidence supporting the involvement of the
5-HT1AR in the effects of psilocybin. Competition binding studies on rodent
brains and primary cells revealed a lack of pronounced selectivity of psilocin
for 5-HT2AR over 5-HT1AR. Nevertheless, the role of the 5-HT2AR remains the
subject of more extensive study and investigation. Ketanserin, a selective
antagonist of the 5-HT2Rs, effectively eliminates head-twitch behavioral
responses in mice; however, it does not attenuate psilocybin-induced structural
modifications in the prefrontal cortex. As a result, uncertainties remain about
whether and how the neuroplastic effects on rescuing disease phenotypes relate
to behavioral responses, especially in humans. Moreover, human studies
investigating the molecular mechanisms of psychedelic-induced plasticity rely on
global parameters such as peripheral BDNF levels, which may not correlate with
the molecular mechanisms occurring in brain cells. For in-depth cellular and
molecular insights into the role of 5-HT2AR, in vitro investigations are
required."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11019282/ [3173]
Using PSCs Schmidt et al (2024) of
the University of Heidelberg showed that psilocin causes 5-HT2A receptor
internalization and redistribution in human cortical neurons, induces BDNF
expression and downstream signaling in human neurons in a dose-dependent manner,
induces gene expression changes associated with axonal and synaptic plasticity,
increases dendritic complexity, and increases synaptic strength and
synaptogenesis.
https://www.researchgate.net/publication/381253376_Psilocin_fosters_neuroplasticity_in_iPSC-derived_human_cortical_neurons
[3175]
Administration of psychedelics to a
relatively small number of people could bring the paralysing stand-off over
Slovenia's past to a quick and elegant halt. The participants would see the
damage they are doing - to themselves and the country - by perpetuating
hostilities against groups and against individuals long dead. They would be able
to more accurately gauge the importance of the historical against the challenges
of the present and future. They would be less susceptible to fearmongering and
superstition. Their nightmares would be put into perspective.
The Slovenians who stand to gain the
most from ranting on about the past for political purposes are the least likely
to have taken them. Among them you will find the most enthusiastic opponents of
the benefits of psychedelics, about which their ignorance resembles what the
average villager in Radenci knows of Tito in the 1940s, i.e. what they have been
told, not what they have experienced.
Unnecessary and counterproductive
rigidity are legal and mental constructs that can be ameliorated by
mind-expanding drugs. They offer a sideways view, and offer users the
opportunity to invite unnecessary and counterproductive rigidity to get lost.
And this is why the anti-drug religion, prohibition, doesn't like them.
Oblivion from alcohol, often
associated with violence, is a legally approved coping mechanism, but is
solipsistic and does nothing to solve the underlying malaises. Drugs other than
alcohol, which can give rise to creative solutions to life stresses or at least
relief by way of euphoria are legally disapproved, and the users accused of
escapism. A drug user is not concerned with his or her genetic predisposition.
They can't change that.
What Slovenia's warring factions need
is not more press stories about what the communists did, but consolation now.
Now does not contain the grudges of the past, nor the anxieties of the future.
Now is not a popular concept for political manipulators. "Now" suggests
something should be done, rather than talked about. "Now" cannot play on
people's resentments and fears. Dealing with "Now" may be financially expensive
compared to promises and grumbling.
Although it is not necessary to
understand the mechanisms of the human brain by which consolation takes place,
and psychedelic people have managed without this so far, it's good to know the
scientists are finally being allowed to fill in the details, and the activation
of 5-HT1A receptors in the anterior cingulate cortex was sufficient to reverse
consolation and sociability deficits in Chinese mandarin voles.
https://elifesciences.org/articles/67638 [302]
The Defence thinks it might work in
Slovenians too.
----------------------------------------------------------------------------
The Englishman stands
for the rights of everyone disadvantaged, discriminated against, persecuted, and
prosecuted on the false or absent bases of prohibition, and also believes the
victims of these officially-sanctioned prejudices have been appallingly treated
and should be pardoned and compensated.
The Englishman requests the return of his CaPs and other rightful property, for
whose distraint Slovenia has proffered no credible excuse or cause.
The Benedictions represent both empirical entities as well as beliefs. Beliefs
which the Defence evidence shows may be reasonably and earnestly held about the
positive benefits of CaPs at the population level, in which the good
overwhelmingly outweighs the bad. Below, the latest version of this dynamic
list.
THE BENEDICTIONS
REFERENCES
TIMELINE OF DRUG LAW v. SCIENCE
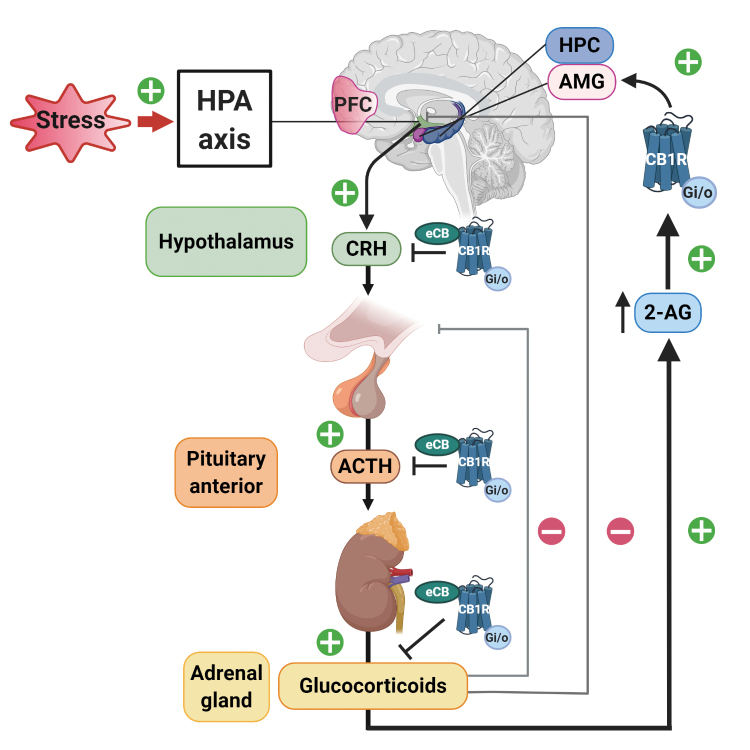
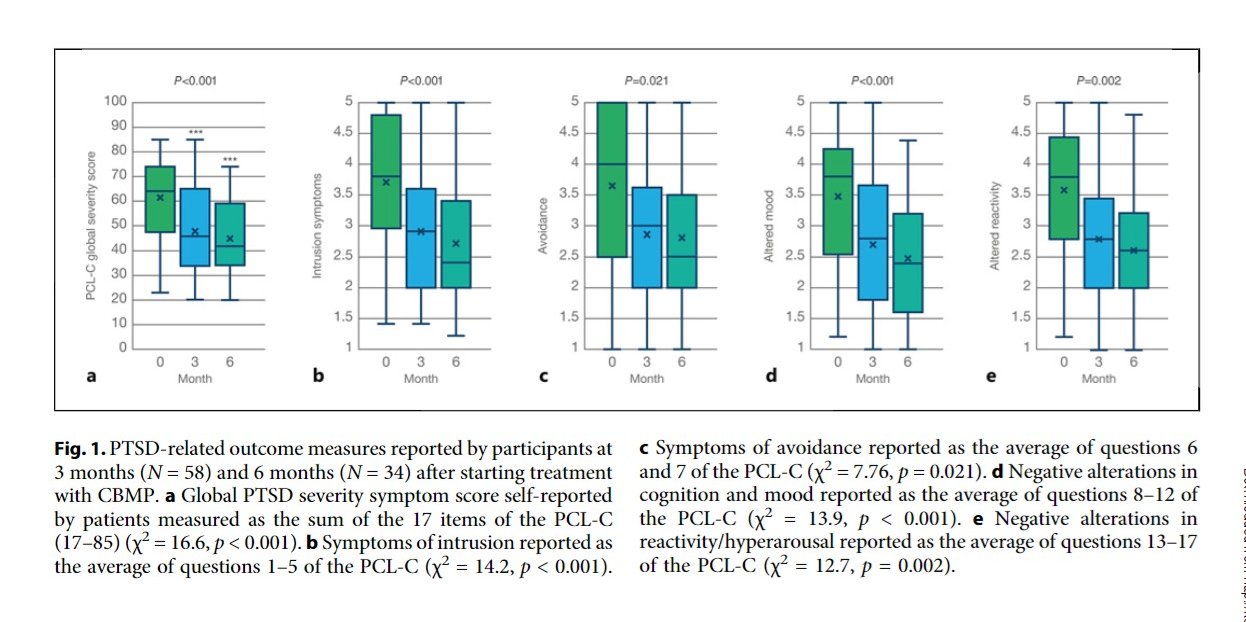
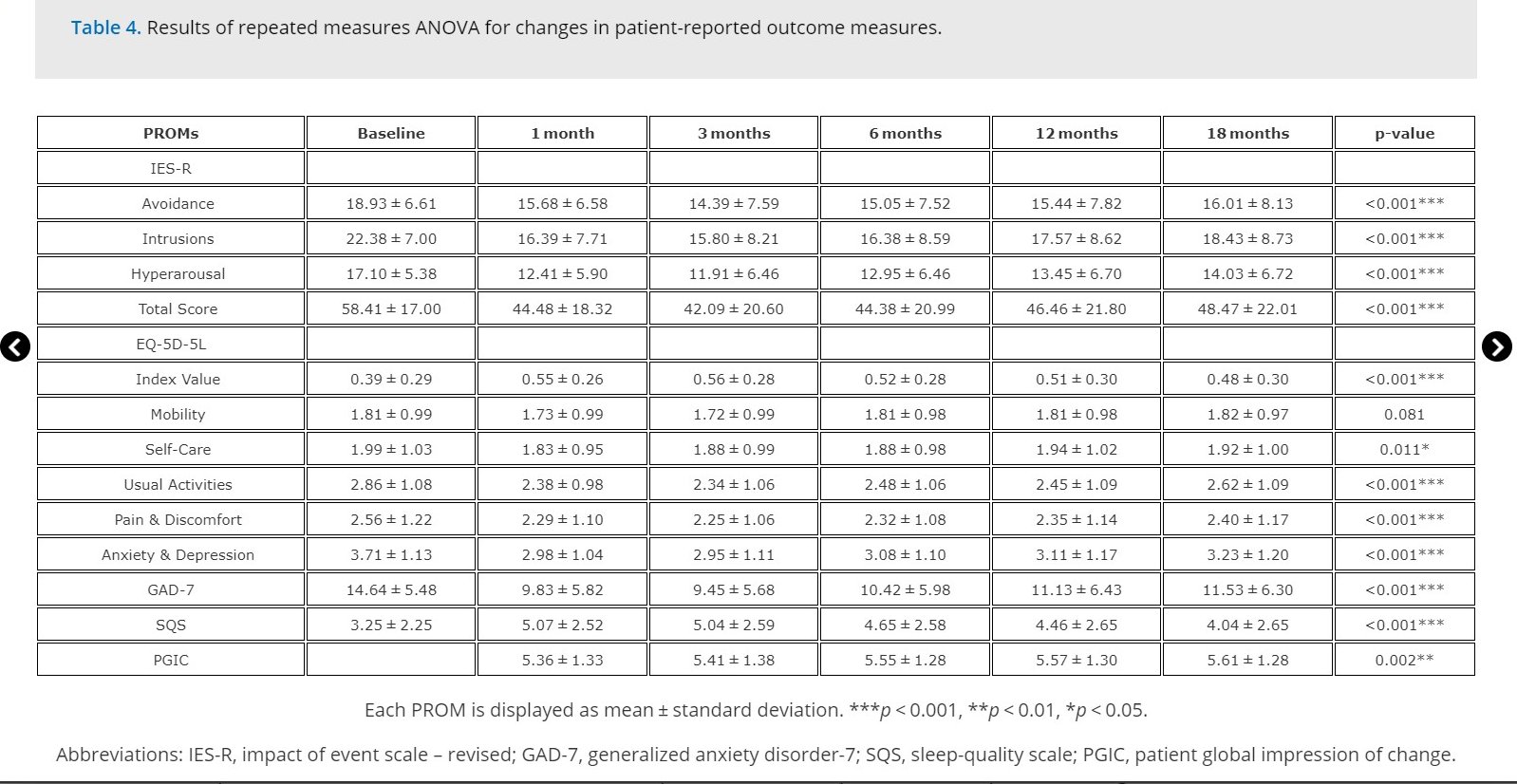
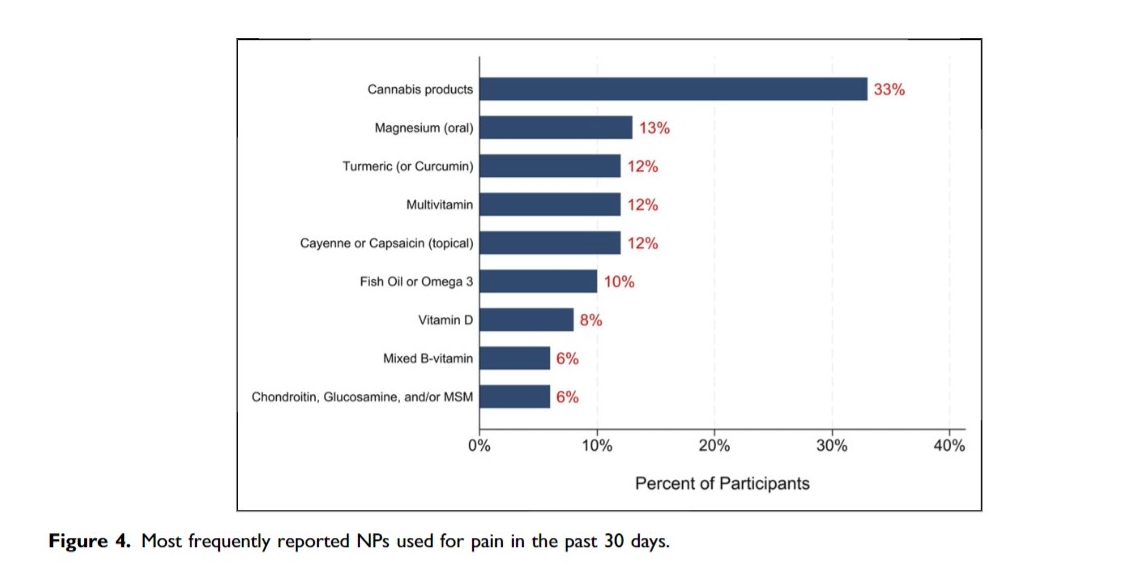
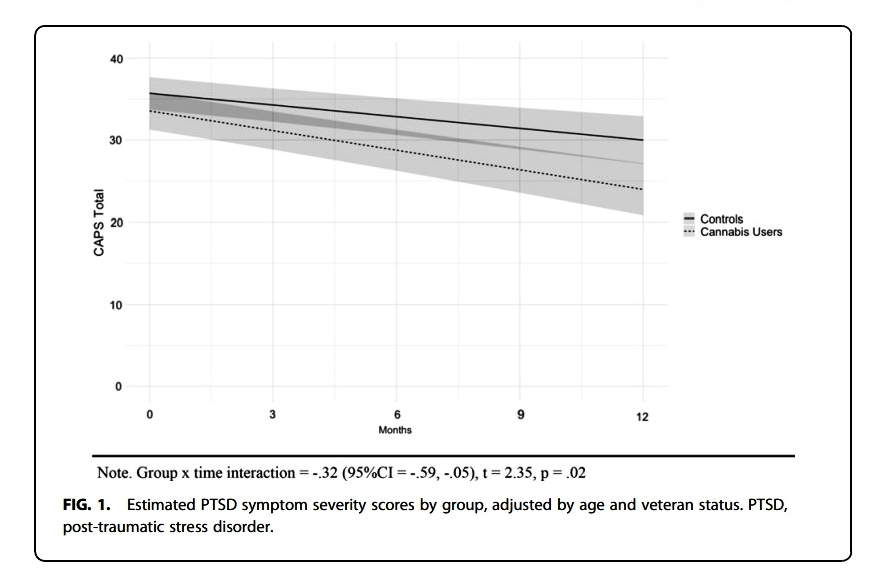
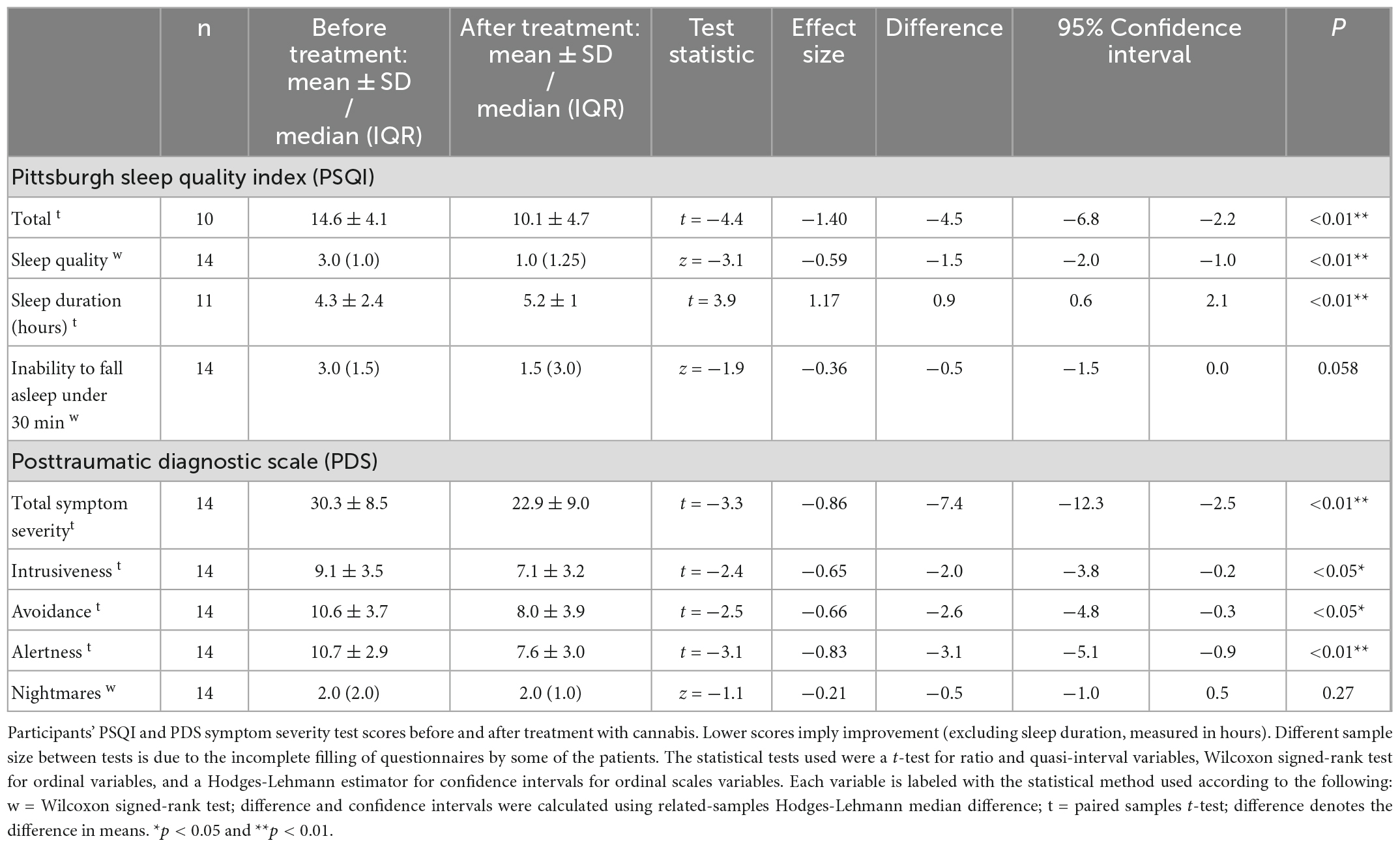
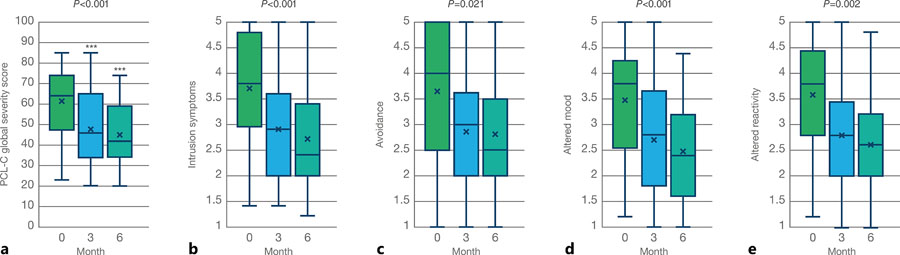
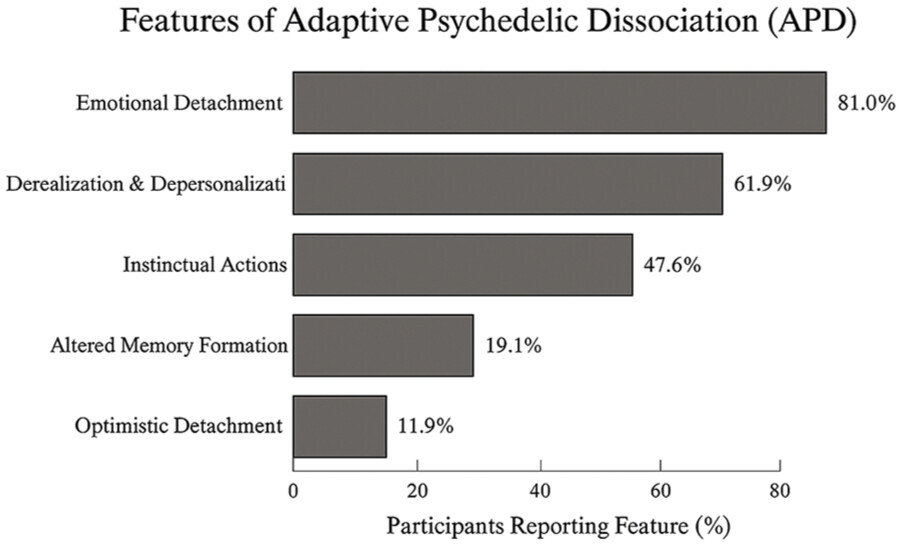
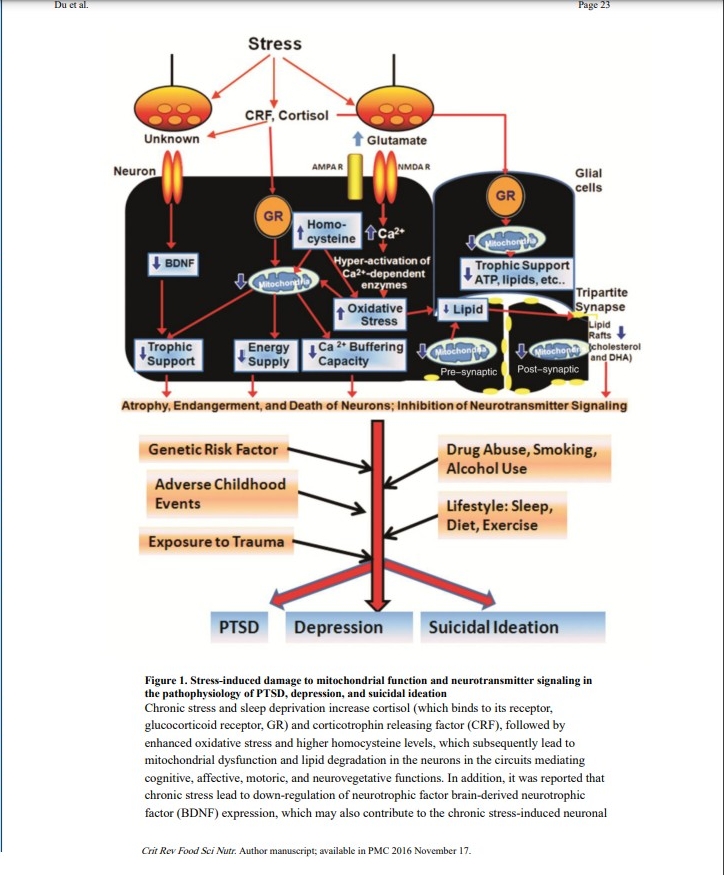
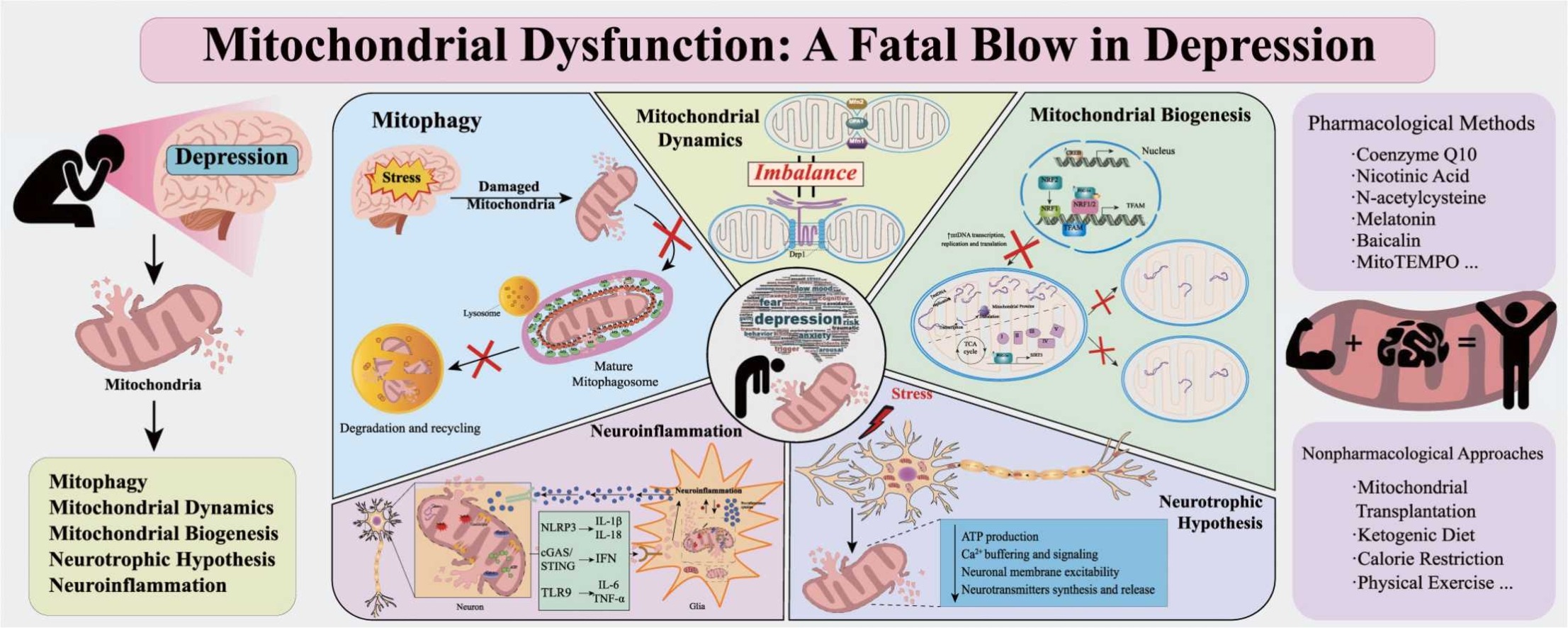
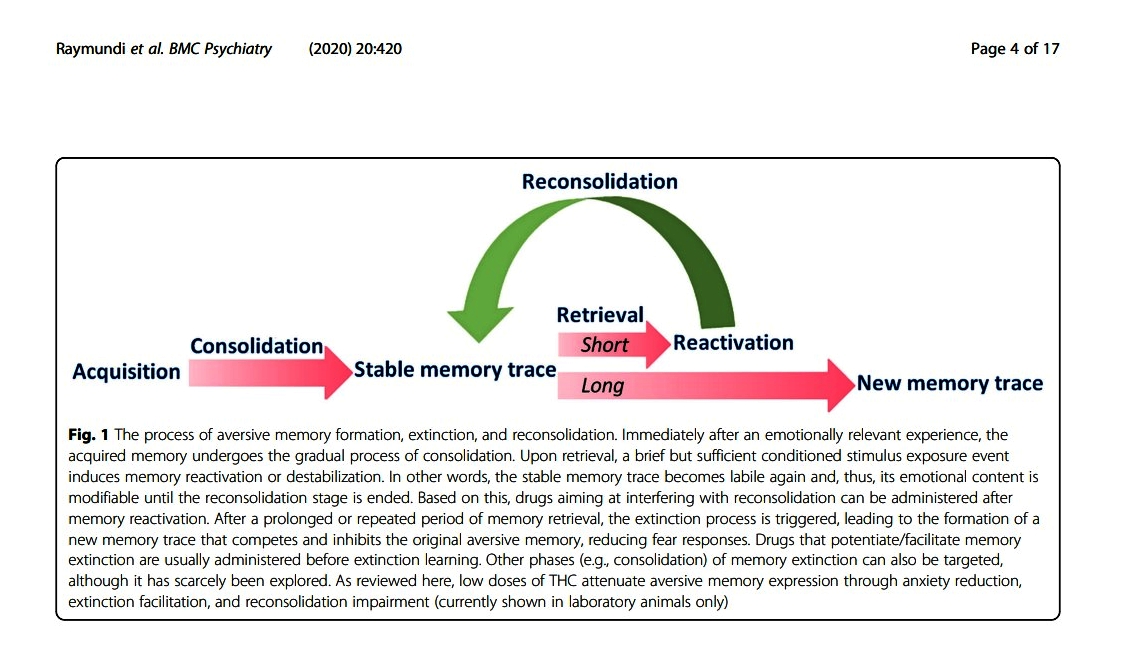
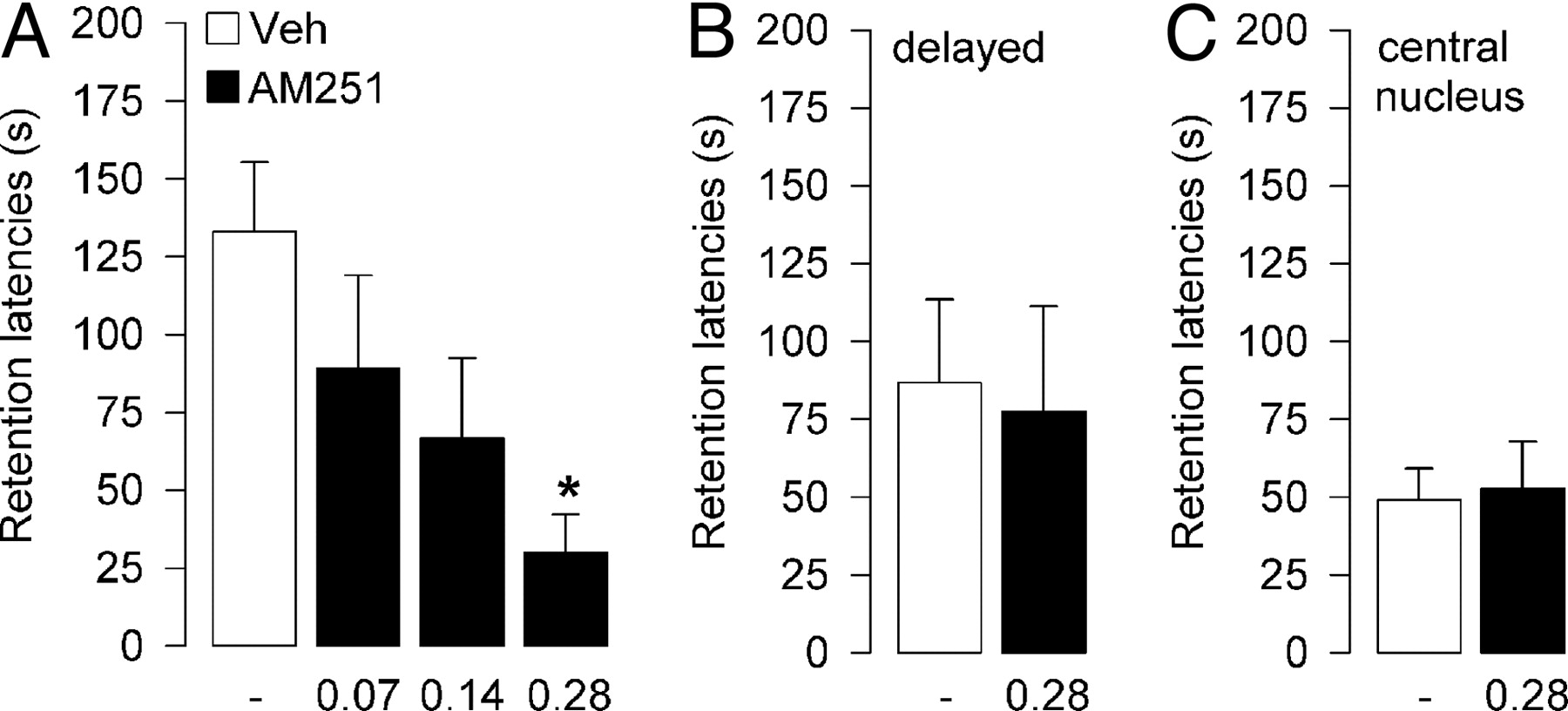
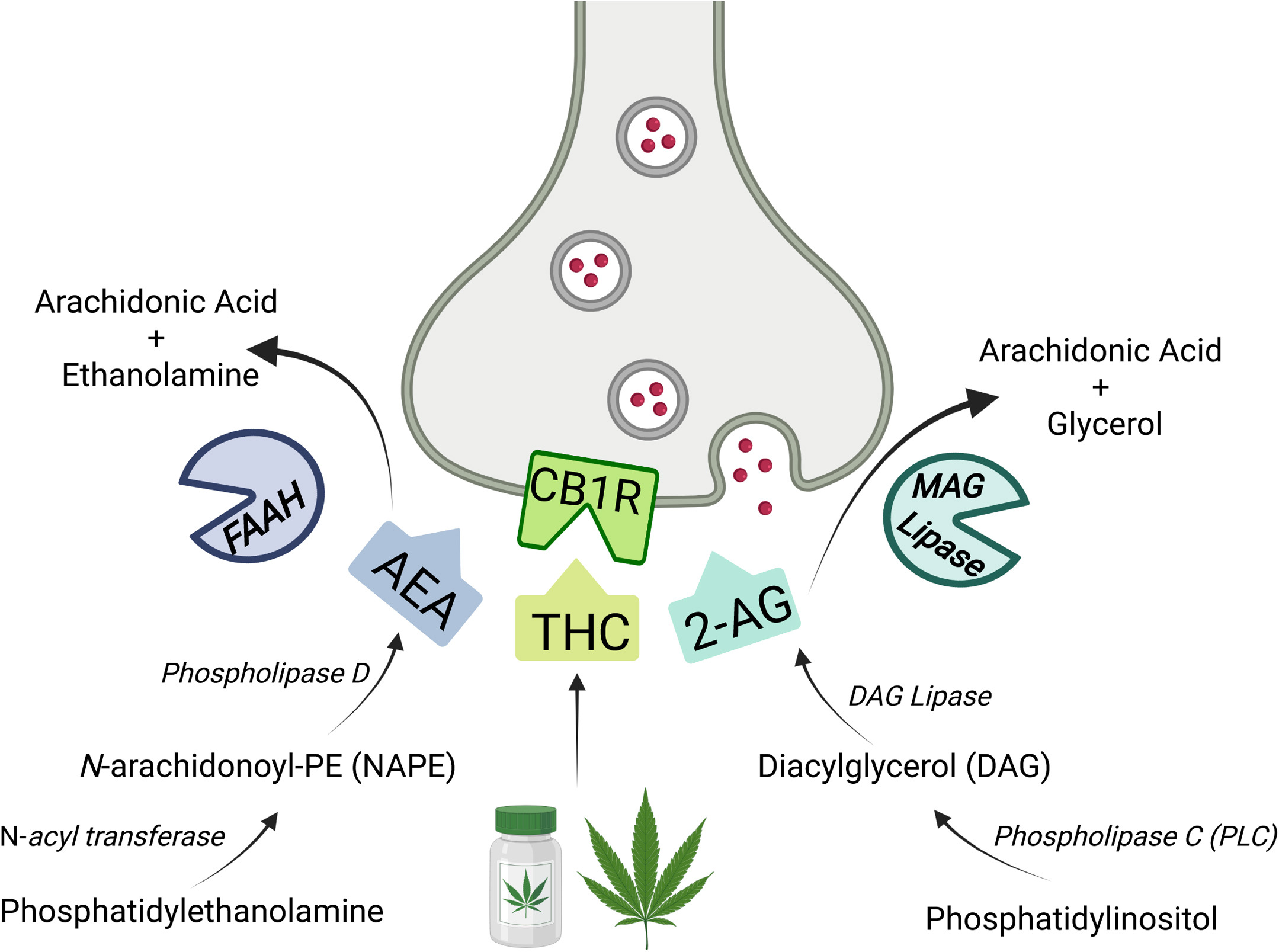
%202490.jpg)