DEPRESSION, CHEMICAL
IMBALANCES CONVENIENT AND OTHERWISE
The Defence agrees with Peter C
Gøtzsche, of the Institute for Scientific Freedom, who writes:
"Psychotropic drugs were developed
based on rat experiments and selected if they disrupt the rat’s normally
functioning brain. The pills don’t cure us, they simply change us by causing a
wide array of effects in people, like all brain active substances do, including
street drugs. And they are not in any way targeted. There is nothing
particularly selective about selective serotonin reuptake inhibitors (SSRIs).
This term was invented by SmithKline Beecham to give paroxetine an advantage
over other drugs, but it was adopted by all companies. There are serotonin
receptors throughout the body, and the drugs have many other effects than
increasing serotonin, e.g. they can affect dopamine and noradrenaline
transmission and can have anticholinergic effects."
And lo and behold, the powers-that-be
have taken control of the language again:
"Psychiatric drugs work...either by
suppressing emotional reactions so that people get numbed and pay less attention
to significant disruptions in their lives or by stimulating them.
"I shall therefore avoid the
conventional nomenclature for drugs. It is misleading to call pills used for
depression antidepressants and pills used for psychosis antipsychotics.
"These drugs are not “anti” some
disease. The 'anti' also gives an association to antibiotics, which save lives,
but psychiatric drugs do not save lives; they take many lives. Furthermore,
unlike antibiotics, they do not have disease specific properties.
"I therefore talk about depression
pills and psychosis pills, which do not give any false promises. "
https://www.scientificfreedom.dk/wp-content/uploads/2023/05/Gotzsche-Critical-Psychiatry-Textbook.pdf
[3021]
The dispensation of depression pills
has increased dramatically since the introduction of SSRIs, on the back of a
surge of advertising based on the notion of chemical imbalance. Since the 1990s,
the number of depressed people with these chemical imbalances has supposedly
gone through the roof.
The idea that depression is a disease
has proved very popular. It's also politically expedient, as approximately half
of the UKs 6m unemployed people of the 1980s stopped being unemployed and were
reclassified as ill instead. Their illness was defined as depression, and how
was their depression defined? By being prescribed depression pills. Simply being
on Prozac, Seroxat or some other SSRI defines you as a victim of "depression".
Yet it turned out there was no
evidence of such a chemical imbalance.
Nowadays, the mental health industry
has taken to claiming they never said people who need pills have a chemical
imbalance, per the serotonin hypothesis. Have you heard this? Did you assume it
was a fact because it came from "on high"? Have you heard any opposing theories?
Ten times psychiatry promoted the
chemical imbalance to the public:
https://x.com/dsowens17/status/1881812105378033897 [3950]
According to a widely reported review
by Moncrieff et al (2022):
"The serotonin hypothesis of
depression is still influential. We aimed to synthesise and evaluate evidence on
whether depression is associated with lowered serotonin concentration or
activity in a systematic umbrella review of the principal relevant areas of
research. PubMed, EMBASE and PsycINFO were searched using terms appropriate to
each area of research, from their inception until December 2020. Systematic
reviews, meta-analyses and large data-set analyses in the following areas were
identified: serotonin and serotonin metabolite, 5-HIAA, concentrations in body
fluids; serotonin 5-HT1A receptor binding; serotonin transporter (SERT) levels
measured by imaging or at post-mortem; tryptophan depletion studies; SERT gene
associations and SERT gene-environment interactions. Studies of depression
associated with physical conditions and specific subtypes of depression (e.g.
bipolar depression) were excluded. Two independent reviewers extracted the data
and assessed the quality of included studies using the AMSTAR-2, an adapted
AMSTAR-2, or the STREGA for a large genetic study. The certainty of study
results was assessed using a modified version of the GRADE. We did not
synthesise results of individual meta-analyses because they included overlapping
studies. The review was registered with PROSPERO (CRD42020207203). 17 studies
were included: 12 systematic reviews and meta-analyses, 1 collaborative
meta-analysis, 1 meta-analysis of large cohort studies, 1 systematic review and
narrative synthesis, 1 genetic association study and 1 umbrella review. Quality
of reviews was variable with some genetic studies of high quality. Two
meta-analyses of overlapping studies examining the serotonin metabolite, 5-HIAA,
showed no association with depression (largest n = 1002). One meta-analysis of
cohort studies of plasma serotonin showed no relationship with depression, and
evidence that lowered serotonin concentration was associated with antidepressant
use (n = 1869). Two meta-analyses of overlapping studies examining the 5-HT1A
receptor (largest n = 561), and three meta-analyses of overlapping studies
examining SERT binding (largest n = 1845) showed weak and inconsistent evidence
of reduced binding in some areas, which would be consistent with increased
synaptic availability of serotonin in people with depression, if this was the
original, causal abnormaly. However, effects of prior antidepressant use were
not reliably excluded. One meta-analysis of tryptophan depletion studies found
no effect in most healthy volunteers (n = 566), but weak evidence of an effect
in those with a family history of depression (n = 75). Another systematic review
(n = 342) and a sample of ten subsequent studies (n = 407) found no effect in
volunteers. No systematic review of tryptophan depletion studies has been
performed since 2007. The two largest and highest quality studies of the SERT
gene, one genetic association study (n = 115,257) and one collaborative
meta-analysis (n = 43,165), revealed no evidence of an association with
depression, or of an interaction between genotype, stress and depression. The
main areas of serotonin research provide no consistent evidence of there being
an association between serotonin and depression, and no support for the
hypothesis that depression is caused by lowered serotonin activity or
concentrations. Some evidence was consistent with the possibility that long-term
antidepressant use reduces serotonin concentration."
https://www.nature.com/articles/s41380-022-01661-0 [2673]
Following this, the serotonin
hypothesis claimed to have made a comeback, but the extent of this amounted to
one person.
https://www.sciencedirect.com/science/article/abs/pii/S0006322322017048
[4080]
madintheuk.com dissects the
conclusions of Erritzoe et al:
"The researchers had three
hypotheses:
"People with depression would have
lower serotonin at baseline than healthy controls.
People with major depressive disorder
would have smaller change in serotonin levels after being dosed with an
amphetamine.
Both baseline serotonin and change in
serotonin levels after amphetamine dosing would be related to the severity of
depression.
"Hypothesis 1
This first hypothesis is the one most
relevant to the bottom-line question: do people with depression have lower
serotonin levels than people without depression?
"To test this, the researchers
conducted a PET scan on the brains of people with depression and healthy
controls. They determined that both the depression group and the control groups
had similar serotonin levels, and both groups were consistent with 'healthy'
levels, which is what previous studies had found. The authors wrote:
"'The regional [serotonin]
distribution for both groups was consistent with previous reports for healthy
individuals with high binding across cortical areas.'
The researchers then ran a bunch of
additional statistical tests on this same data (tests to include other factors,
such as age, and then breaking the data down into specific regions and
re-running the tests—a controversial statistical process known as p-hacking
because it increases the likelihood of finding a statistically significant
result by chance). Even after all this, the researchers found that the
depression group and the healthy control group continued to have serotonin
levels which were no different, except for one slight average difference in one
brain region (the temporal cortex). Even in this area, the data shows an almost
complete overlap between the two groups.
"Conclusion number one: There was no
difference in serotonin levels between those with depression and those without.
Their first hypothesis was demonstrated to be false.
"Hypothesis 2
The second element of the study was a
test to see whether a dose of amphetamine, which is known to trigger the release
of serotonin, would produce less of a response in depressed patients than in the
controls.
"The researchers dosed all
participants with 0.5 mg/kg of d-amphetamine, and measured how much, on average,
each group’s levels of serotonin changed. This was done by measuring serotonin
binding potential in the frontal cortex, to estimate serotonin release capacity.
"They found a statistically
significant effect: on average, the healthy control group’s serotonin levels
changed more than the serotonin levels of those with a diagnosis of major
depression after being dosed with an amphetamine. This was the result that
prompted the researchers to write that their study 'provides clear evidence for
dysfunctional serotonergic neurotransmission in depression by demonstrating a
reduced 5-HT release capacity in patients undergoing a major depressive
episode.'
"There was in fact a wide variation
in serotonin release in both the depressed patients and the controls. And if the
serotonin response for each of the individuals is plotted out on a graph, as was
done in the paper, it immediately becomes apparent that the 'statistically
significant' effect arises from two individuals: one in the depressed group
without Parkinson’s, and one in the depressed group with Parkinson’s.
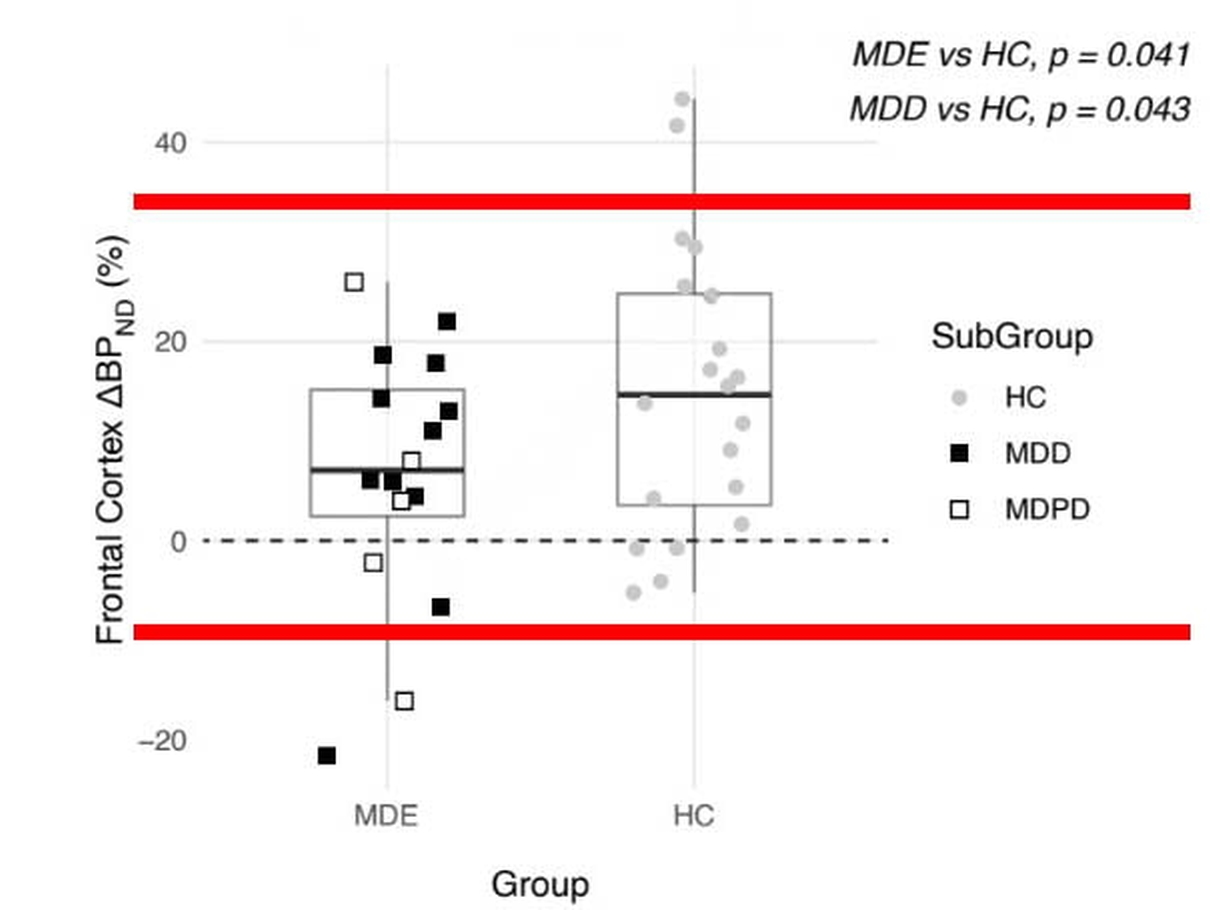
"In the chart below (from the study
publication, red bars added), the depression group scores are on the left, while
the control group scores are on the right. The black boxes in the depression
group are for those without Parkinson’s; the white boxes for those with
Parkinson’s.
"As can be seen, there are two
outliers (one black box and one white box), and except for those two, every
depressed person’s score, detailing how much their serotonin levels changed,
overlaps with a healthy person’s score.
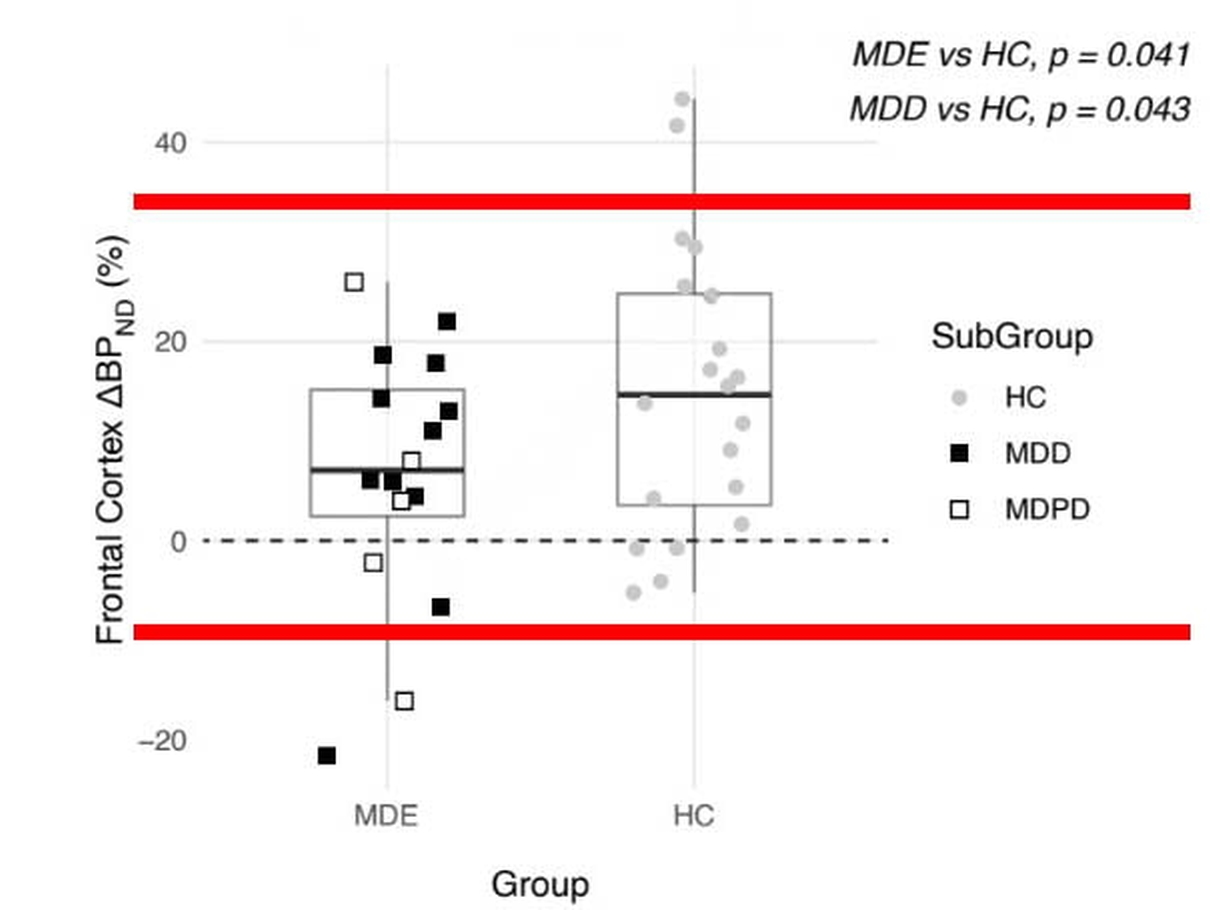
"Since Parkinson’s disease is an
obvious confounder, there is only one outlier in the depressed group, out of 11.
"The researchers, as they reported
their results, ignored this fact. Instead, they calculated the mean change in
serotonin release scores for the 20 healthy controls and 16 depressed patients,
and concluded that there was a slight 'statistically significant' difference (p
value = .041). Without the one outlier, this statistically significant finding
would have vanished.
"Such is the data related to
hypothesis number two. And here is the relevant conclusion to draw: In 10 of 11
depressed patients without Parkinson’s, their serotonin release scores
overlapped with those of the healthy controls, and thus were in a normal range.
Four out of five in the Parkinson’s group were within this same normal range.
"Hypothesis 3
To test their third hypothesis, the
researchers ran an analysis to test whether serotonin levels were related to the
severity of depression, measured by the Hamilton Depression Rating Scale
(HAM-D), in both those with depression and those with depression and Parkinson’s
disease). They found that severity of depression across both groups was not
related at all to levels of serotonin.
"Then they ran a similar analysis to
test whether the change in serotonin levels in response to the amphetamine
dosing was related to the severity of depression. They found that severity of
depression was not related to the change in levels of serotonin either."
"'There was no significant
correlation between HAM-D depression scores and baseline [serotonin],' the
researchers wrote. They added, 'There were no statistically significant
associations between HAM-D depression scores and [change in serotonin].'
"Thus, their third hypothesis—that
serotonin levels or change in serotonin would be related to depression
severity—was also proven false.
"They write, 'We found no
relationship between the severity of depression (as assessed by a HAM-D scale)
and the magnitude of induced 5-HT release. At this stage we have no explanation
for the lack of such relationship.'"
https://www.madintheuk.com/2022/11/serotonin-depression-myth/?utm_source=ReviveOldPost&utm_medium=social&utm_campaign=ReviveOldPost
[4083]
This represents a split in thinking
between the disease-based model of depression and a rather different philosophy
of life which might be described as psychiatry-skeptic. Important criticisms of
this psychiatric world-view took shape with Thomas Szasz and his 1960 book "The
Myth Of Mental Illness" and the Goldenhan experiment - the latter described as
the research from which psychiatry never fully recovered.
Around the same time the use of
psychedelics became popular, and then illegal. People took them to alter their
mood, and it wasn't intended to make them depressed.
Despite this, the connection was not
made, in the public imagination, between LSD and depression. Serotonergic
psychedelics were marched off into a fantastical "narcotics" category.
Instead the disease-based, and
therefore drug-based, model of mental illnesses - for the major categories of
which, schizophrenia, psychosis, depression, no consistent evidence of any
metabolic or biochemical marker has ever been shown - persisted and remained
dominant into the era of SSRIs and continues to be supported by, of course, the
pharmaceutical manufacturers right up to the present. There was every reason to
hope, of course, that finding chemical pathways to alter would lead to cure. But
ever since the era of haloperidol and benzodiazepam, the truth was that "drugs
that diminish people's responsiveness to their environment in general can cause
people who are in a psychotic state to lose interest in their delusional
preoccupations" (Deniker, 1960, in The past and future of psychiatry and its
drugs - Moncrieff, J. (2020) BPS Psychotherapy Section Review, No. 65, Winter
2020, 77-83). Psychiatry was having trouble maintaining its respectability and
professional self-respect, and it was having trouble keeping up with other, more
successful branches of medicine, which did indeed find plausible and effective
mechanisms of drug action in scientifically demonstrable metabolic dysfunctions
(Moncrieff, ibid.)
https://discovery.ucl.ac.uk/id/eprint/10137711/3/Moncrieff_The%20past%20and%20future%20of%20psychiatry%20and%20its%20drugs.pdf
[1368]
"She argues that, given how little we
know about the biology of mental illness, there are no targeted,
disease-specific drugs; antidepressants are closer in nature to alcohol. They do
not rectify an underlying brain malfunction, but rather change how you think or
feel. 'Those changes are superimposed onto whatever someone is thinking and
feeling at the time. We even have an expression for this with alcohol: we talk
about "drowning your sorrows"' Moncrieff said, when we met in her spartan shared
office at King’s College. 'If you recognise that’s what the drugs are doing,
then it immediately becomes obvious they are not going to be a long-term
solution and they might be harmful.'"
and
"'The pharmaceutical industry and the
medical profession have coached the population for decades that there is a
medical solution to various crises in life – and I think we need to uncage
people because that’s simply not true,' Moncrieff said. 'We need to find more
non-medical ways of supporting people through crises.' Rather than viewing
depression as an illness, she wants people to see it as a 'mood state': 'Mood
states are related to emotions, and moods and emotions are the way that human
beings, which are complex, intelligent organisms, respond to events in their
environment. Depression is by definition a reaction to a state that someone
doesn’t want to be in, to something that’s gone wrong in someone’s life, or a
stressful situation.'"
https://web.archive.org/web/20230422110709/https://www.newstatesman.com/the-weekend-interview/2023/04/joanna-moncrieff-im-not-convinced-antidepressants-have-any-use
[2455]
"Moncrieff is clear there is no shame
in suffering from mental illness. But she believes the best approach to tackling
it is through talking therapies, exercise and a willingness to make appropriate
changes in one’s life. 'But a very neuro-reductionist view of mental health
problems and life in general is particularly gaining traction among young
people. It trumps everything else. Why have marital therapy if your brain is the
problem?'"
https://archive.ph/2025.01.12-003252/https://www.thetimes.com/uk/society/article/do-antidepressants-work-british-professor-depression-medication-ld28kgvj5#selection-3603.0-3603.437
[3898]
Various critics with ties to
pharmaceutical companies lined up to criticise her debunking of the serotonin
hypothesis.
"Responding to the criticism, Prof
Moncrieff said the aim of the study was not to argue that antidepressants don’t
work but to question whether the pills should be prescribed in the first place.
"'People are told the reason they
feel depressed is that there is something wrong with the chemistry in their
brain and antidepressants could put it right. But if there’s no evidence there’s
anything wrong with the brain’s chemistry, then that doesn’t sound like a
sensible solution. This profession has misled people for so long about the need
for antidepressants and now doctors don’t want to admit they got it wrong.’"
https://www.dailymail.co.uk/health/article-11042143/Joanne-Moncrieff-University-College-London-disproves-link-low-serotonin-depression.html
[4194]
The problem was elucidated in 2016 by
Robin M Murray, Professor of Psychiatric Research at the Institute of
Psychiatry, King’s College London (KCL) and a Fellow of the Royal Society, who
discusses his journey in "Mistakes I Have Made in My Research Career", under
such headings as "The Unrewarding Search for the Causes of the Brain Changes
Underlying Schizophrenia", "The Runaway Rise of the Neurodevelopmental
Hypothesis", "I Ignored Social Factors for 20 Years", and "Dopamine
Supersensitivity; Another Old Idea I Dismissed for too Long",
"If I had the chance to have a second
career, I would try harder not to follow of the fashion of the herd. The
mistakes I have made, at least those into which I have insight, have usually
resulted from adhering excessively to the prevailing orthodoxy. Fortunately, I
have often been rescued from this by the arrival of a brilliant young research
fellow who has proposed a novel approach; I have usually resisted her/his idea
initially before eventually come round to its merits. Sadly, this reliance on
the corrective influences of younger colleagues has its limits. For example,
David Marsden was already a famous professor when I met him; he must have been
too senior for me to take seriously his insightful comments on the effects of
antipsychotics on the brain! Consequently, I sailed on, believing the same false
dogma for several decades.
"It is curious that as I grow older,
I find myself increasingly asked to give my predictions for future directions in
psychiatry. This is likely to be as productive as asking Mick Jagger to comment
on likely new trends in Hip-Hop. I shall therefore confine myself to saying that
if I was starting afresh, I would throw myself into examining gene × environment
interactions and epigenetics, as ways of elucidating the mechanistic pathways
through which the environment contributes to the onset of psychosis. However,
one has to be very good at statistics to succeed in this area. So if I wasn’t
clever enough, I would instead go into neurochemical imaging; it is true that
the maths is still complicated but at least the pictures of the brain are
pretty.
"I expect to see the end of the
concept of schizophrenia soon. Already the evidence that it is a discrete entity
rather than just the severe end of psychosis has been fatally undermined.
Furthermore, the syndrome is already beginning to breakdown, for example, into
those cases caused by copy number variations, drug abuse, social adversity, etc.
Presumably this process will accelerate, and the term schizophrenia will be
confined to history, like 'dropsy.'"
https://academic.oup.com/schizophreniabulletin/article/43/2/253/2730504?login=false
[4327]
Let's take a moment to look at one
widely-touted cure-all, benzodiazepines.
"'It's more difficult to withdraw
people from benzodiazepines than it is from heroin – it just seems that the
dependence is so ingrained and the withdrawal symptoms you get are so
intolerable that people have a great deal of problem coming off. The other
aspect is that with heroin usually the withdrawal is over within a week or so.
With benzodiazepines a proportion of patients go on to long-term withdrawal and
they have very unpleasant symptoms for month after month and I get letters from
people saying that it can go on for 2 years or more. Some of the tranquilliser
groups can document people who still have symptoms 10 years after stopping.'
(Source: Professor Malcolm Lader, BBC Radio 4, Face the Facts, broadcast on
March 16, 1999)."
“'All the benzodiazepines are
non-selective and act on all types of GABA/benzodiazepine receptors. Valium acts
on exactly the same receptors as Klonopin etc. The main reason that
benzodiazepines have somewhat different structures is not so much that they act
on different receptors (they don't) but so that the drug companies can call them
different drugs.'"
http://www.benzo-case-japan.com/addiction-english.php [1766]
Maust et al (2023) at the University
of Michigan at Ann Arbor reported in JAMA that ceasing benzodiazepine use was
associated with an increased risk of dying. Among people who weren't
simultaneously taking an opioid, the adjusted cumulative incidence of death over
1 year was 5.5% for those who stopped benzodiazepine treatment compared with
3.5% for those who didn't.
Discontinuation was defined as having
no benzodiazepine prescription for 31 consecutive days during a 6-month period
after baseline. Patients were followed for about 1 year after baseline
benzodiazepine prescriptions.
The researchers also found the risks
of secondary outcomes including nonfatal overdose, suicidal ideation, and
emergency department use were higher among those who stopped benzodiazepines,
whether or not they also used opioids (relative risk 1.2, 1.4, and 1.2,
respectively).
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2813161?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamanetworkopen.2023.48557
[4278]
Prisoners force-fed Librium in 1961
became addicted after two months, says Professor Malcolm Lader.
Says Professor Heather Ashton:
"We had people who'd been told they
had multiple sclerosis, and when we got them of the benzos their symptoms
disappeared."
"It was very difficult to get
compensation because nobody realized it was a real illness."
Both Lader and Ashton put research
proposals to the Medical Research Council and the Wellcome Trust, with a sample
of 300 long-studied participants, MRI, EEG and magnetoencephalography, but they
never got the money for it.
In 2014, drug poisonings with
benzodiazepines reached 15385 in England, more than all illegal drugs combined.
Heroin: 2450, cocaine: 2306, and by some classification somehow, cannabis 739.
Deaths (England and Wales) were heroin: 952, methadone 394, benzodiazepines 372,
and diazepam/valium 258.
https://www.youtube.com/watch?v=MVoFlGR7Lhs [1767]
In Scotland
"In 93% of all drug misuse deaths,
more than one drug was found to be present in the body.
"Of all drug misuse deaths in 2021,
84% involved opiates or opioids (such as heroin, morphine and methadone). 69%
involved benzodiazepines (such as diazepam and etizolam).
"In recent years there has been a
large increase in the number of drug misuse deaths involving benzodiazepines. In
2015 there were 191 of these deaths and in 2021 there were 918; almost five
times as many. This increase has mostly been driven by street benzodiazepines
rather than those which are prescribed.
"In 2020 (the most recent year
available for the rest of the UK) Scotland’s drug misuse rate was 3.7 times that
for the UK as a whole, and higher than that of any European country."
and
"The proportion of drug misuse deaths
where gabapentin and/or pregabalin were implicated has increased from <1% in
2008 to 36% in 2021. These are drugs used to treat epilepsy and nerve pain. The
proportion where cocaine was implicated has also increased from 6% in 2008 to
30% in 2021. The number of drug misuse deaths where alcohol was implicated (in
addition to a controlled drug) has remained fairly similar, although the
proportion has fallen from 29% in 2008 to 12% in 2021."
The report, "Drug-related deaths in
Scotland in 2021" does not mention cannabis, marijuana, psychedelics, LSD,
psilocybin or mushrooms.
https://web.archive.org/web/20240323190516/https://www.nrscotland.gov.uk/files/statistics/drug-related-deaths/21/drug-related-deaths-21-report.pdf
[2607]
Benzos have even spawned their own
disease syndrome:
"Benzodiazepine-induced neurological
dysfunction (BIND) has been proposed as a term to describe symptoms and
associated adverse life consequences that may emerge during benzodiazepine use,
tapering, and continue after benzodiazepine discontinuation."
Ritvo et al's Table 1 of their
"Long-term consequences of benzodiazepine-induced neurological dysfunction: A
survey" (2023) shows the symptoms reported, which occurred across all
respondents, regardless of taper status and cause for original prescription of
the benzodiazepine.

https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0285584
[2821]
Eventually the late Professor Ashton,
realizing that the patients knew better what was going on than their doctors,
published an online manual on how to withdraw from benzodiazepines. The manual
is available in twelve languages and Slovene is not one of them.
https://benzo.org.uk/manual/contents.htm [1768]
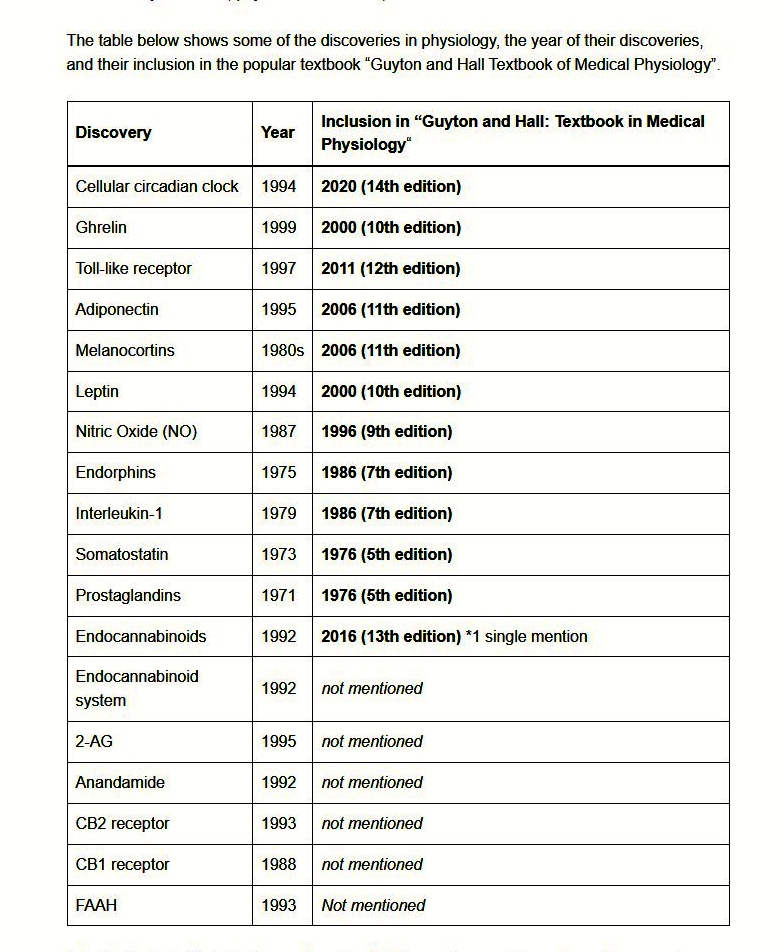
Clozapine, an atypical antipsychotic
drug, is a tricyclic dibenzodiazepine derivative,
8-chloro-11-(4-methyl-1-piperazinyl)-5H-dibenzo [b,e] [1,4] diazepine.
Despite having been withdrawn in
other countries, clozapine is still in the Slovenian pharmacopoeia.
http://www.cbz.si/cbz/bazazdr2.nsf/o/26D48494772FCCCCC12586880005AB9A?opendocument
[4349]
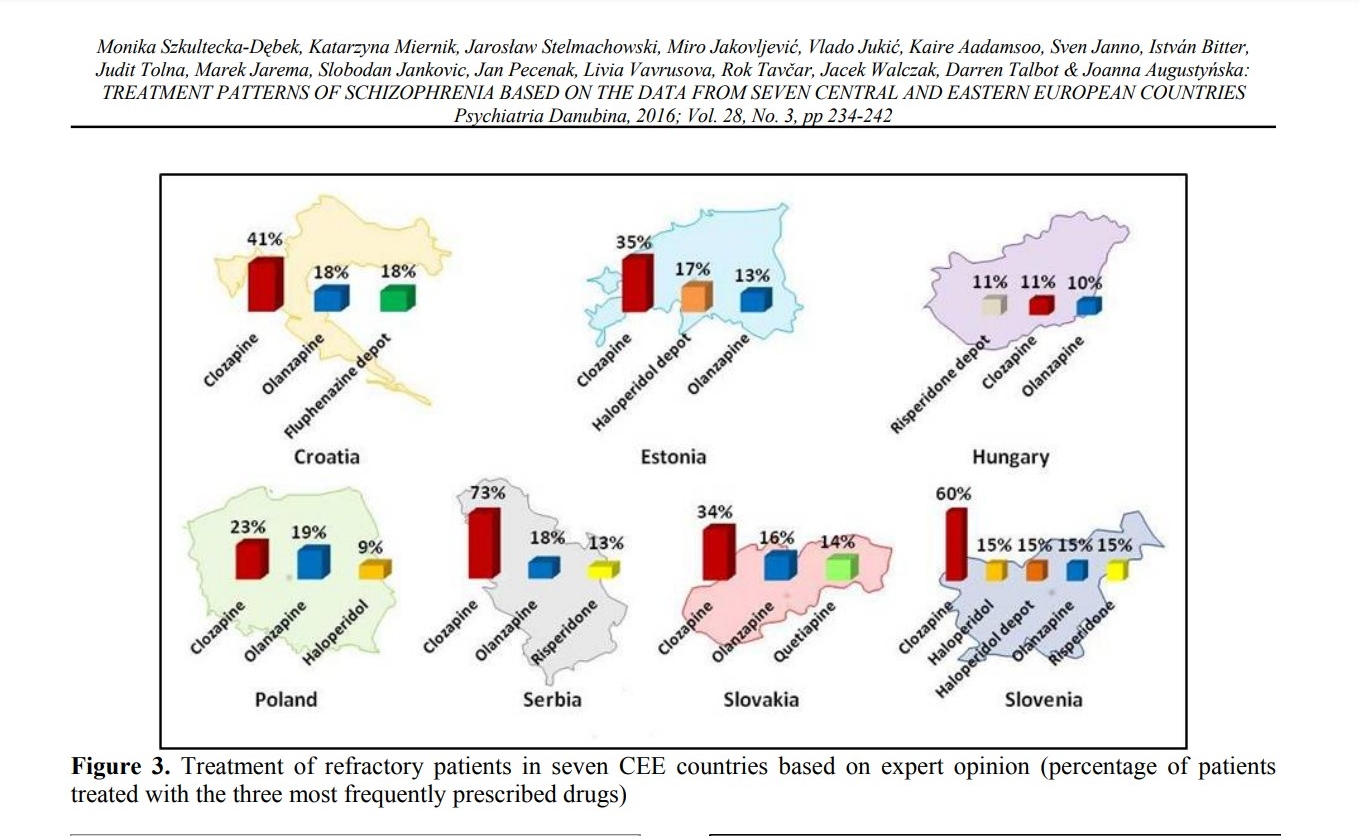
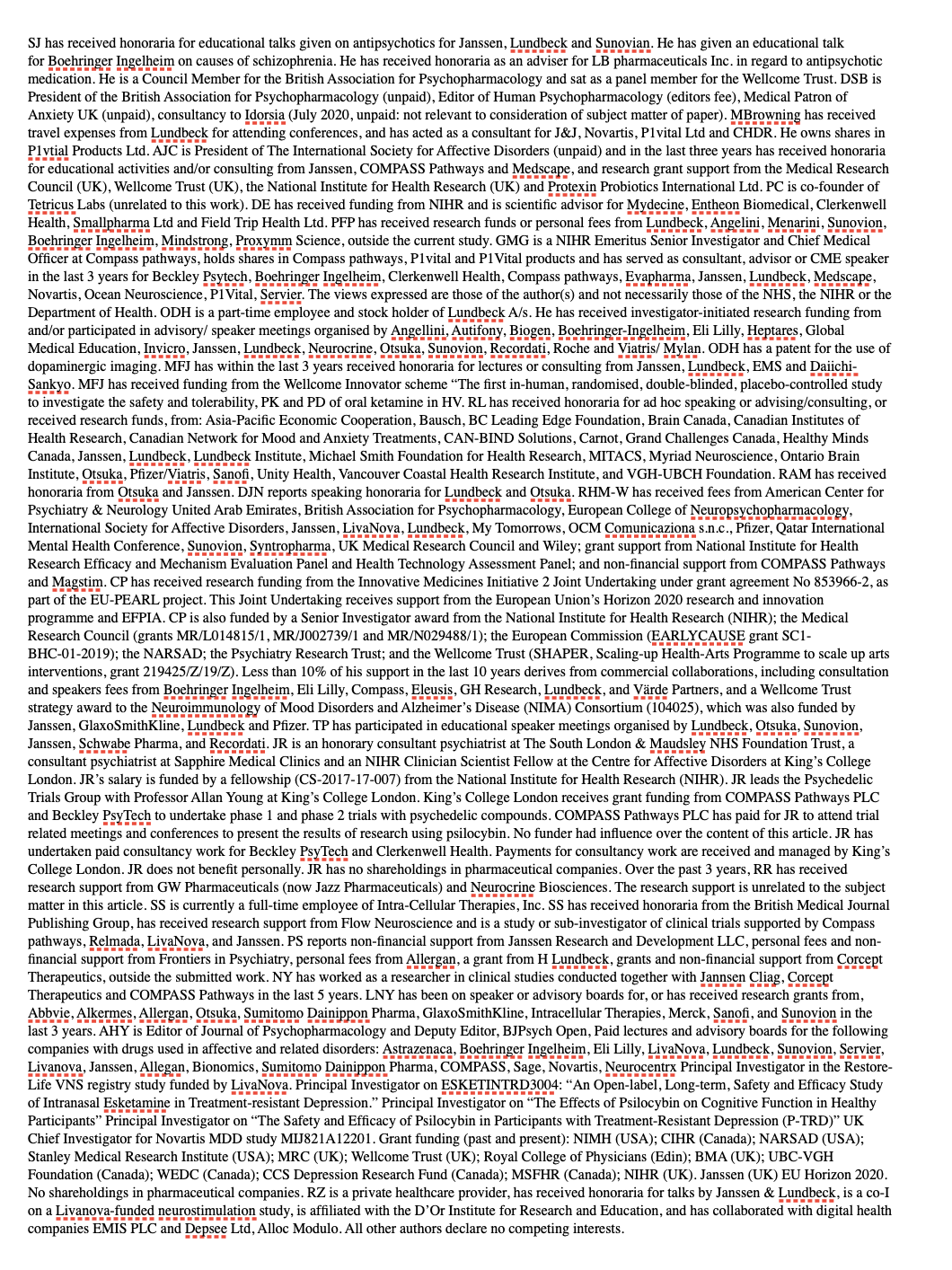
Szkultecka-Debek et al have some
information on drug choices in schizophrenia in CEE countries:
Clozapine was the most reported
medication for refractory patients. No clozapine deaths had been recorded in
Slovenia as of 2016.
https://www.psychiatria-danubina.com/UserDocsImages/pdf/dnb_vol28_no3/dnb_vol28_no3_234.pdf
[4351]
Describing clozapine as an
"outstanding drug", a newer study, "An expert review of clozapine in Eastern
European countries: Use, regulations and pharmacovigilance", a newer study, by
Sagud et al (2023) found wide disparities:
"Clozapine prescription among
antipsychotics in 2021 varied six-fold across countries, from 2.8 % in the Czech
Republic to 15.8 % in Montenegro. The utilization of antipsychotics in both 2016
and 2021 was highest in Croatia, and lowest in Serbia in 2016, and Montenegro in
2021, which had half the defined daily dose (DDD)/1000/day compared to the
Croatian data. From 2016 to 2021, the prevalence of antipsychotic use increased
in almost all countries; the proportion of clozapine use mainly remained
unchanged. Differences were detected in hematological monitoring requirements
and clozapine approved indications. Only a few national schizophrenia guidelines
mention clozapine-induced myocarditis or individual titration schemes. The
VigiBase search indicated major underreporting regarding clozapine and its fatal
outcomes. By comparison, the United Kingdom had less than half the population of
these Eastern European countries but reported to VigiBase more clozapine ADRs by
89-fold and clozapine fatal outcomes by almost 300-fold."
https://www.sciencedirect.com/science/article/abs/pii/S0920996423003122?via%3Dihub
[4352]
Then, according to a January 2024
report in the Times, it was reported "this outstanding drug" has been
"linked to 7,000 deaths since it was
approved.
"The Times found that the drug is
linked to almost eight times as many reported deaths as any other high-risk
medicine.
and
"The Times’ analysis shows an average
of more than 400 clozapine-linked deaths have been reported to the Medicines and
Healthcare products Regulatory Agency each year for the past decade.
"The medicines watchdog’s yellow card
reporting scheme also gets around 2,400 notifications a year of 'suspected
serious reactions' to the drug."
and the side-effects are
"Blood disorders: signs of problems
include flu-like symptoms such as sore throat and temperature.
"Seizures.
"Heart disease: signs of a problem
include chest pain, palpitations, or a rapid pulse.
"Diabetes: a third of people taking
clozapine may develop diabetes after five years of treatment, the majority of
these cases happen within the first six months.
"Bowel obstruction: clozapine can
cause slowing of bowel movement resulting in constipation, blockage and a
'paralytic ileus', which may be fatal.
"Skin reactions: people taking
antipsychotics may be more sensitive to sunlight. You should consider how to
protect people’s skin from direct sunlight."
https://www.standard.co.uk/news/health/what-clozapine-prescription-drug-dangerous-side-effects-b1131180.html
[4348]
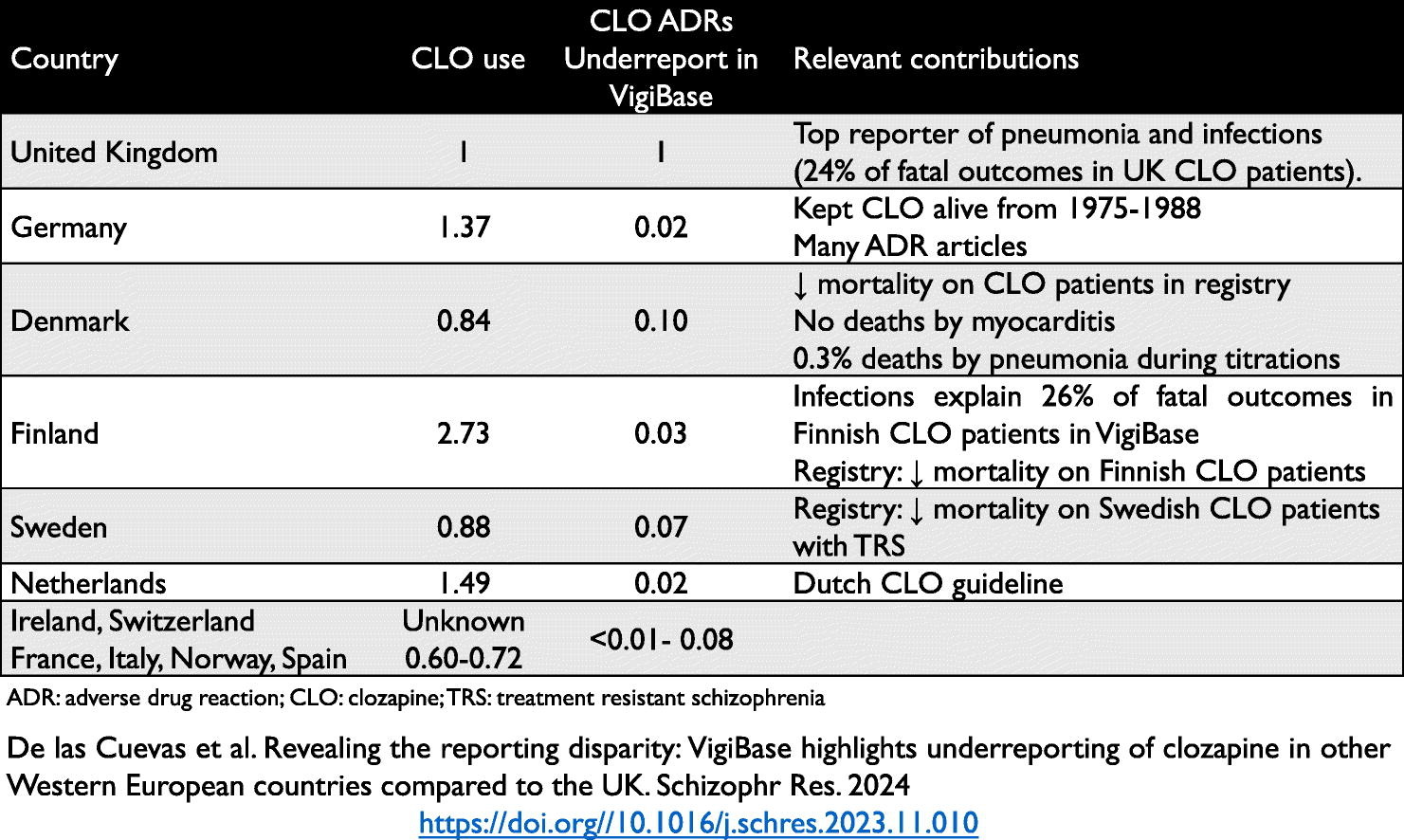
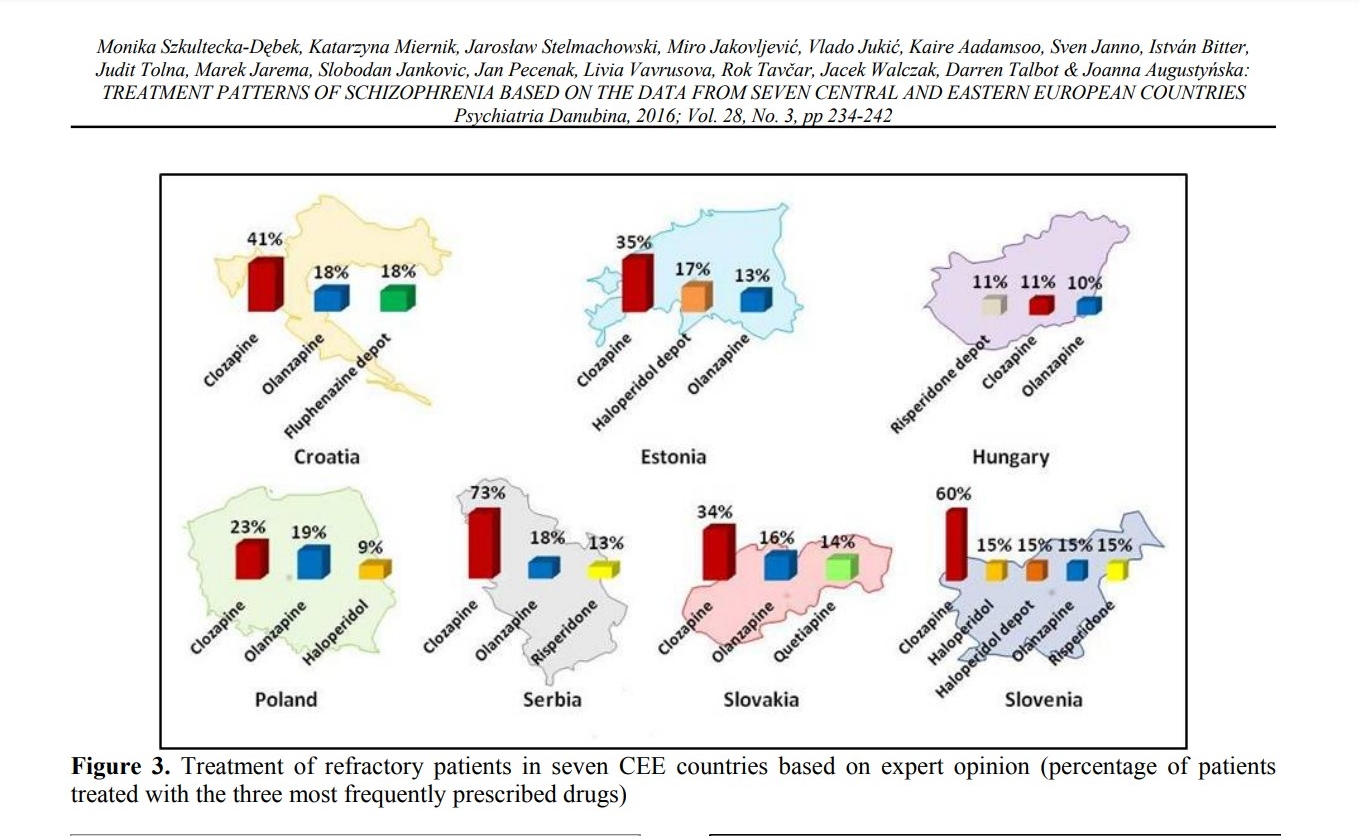
The month prior saw the publication
of "Revealing the reporting disparity: VigiBase highlights underreporting of
clozapine in other Western European countries compared to the UK" by De las
Cuevas et al (2023) wherein:
"VigiBase reports from clozapine's
introduction to December 31, 2022, were studied for ADRs and the top 10 causes
of fatal outcomes. The UK was compared with 11 other top reporting Western
countries (Germany, Denmark, France, Finland, Ireland, Italy, Netherlands,
Norway, Spain, Sweden and Switzerland). Nine countries (except Ireland and
Switzerland) were compared after controlling for population and clozapine
prescriptions.
"Results
The UK accounted for 29 % of
worldwide clozapine-related fatal outcomes, Germany 2 % and <1 % in each of the
other countries. The nonspecific label “death” was the top cause in the world
(46 %) and in the UK (33 %). “Pneumonia” was second in the world (8 %), the UK
(12 %), Ireland (8 %) and Finland (14 %). Assuming that our corrections for
population and clozapine use are correct, other countries underreported only
1–10 % of the UK clozapine fatal outcome number.
"Conclusions
Different Western European countries
consistently underreport to VigiBase compared to the UK, but have different
reporting/publishing styles for clozapine-related ADRs/fatal outcomes. Three
Scandinavian registries suggest lives are saved as clozapine use increases, but
this cannot be studied in pharmacovigilance databases."
https://www.sciencedirect.com/science/article/pii/S092099642300422X?via%3Dihub
[4350]
But it seems this bad news about
clozapine wasn't really news at all, according to psychiatric patient Zekria
Ibrahimi, in response to the BMJ article "Coroners warn health secretary of
clozapine deaths" (2019):
"Clozapine was first produced in
1958. It was marketed from 1970. It began killing patients. After multiple
deaths in Finland, it was banned there, and then across Europe. The major
problem was 'agranulocytosis'. The BMJ feature mentions agranulocytosis among
other side effects, without emphasizing agranulocytosis as the prime key danger.
"Research on clozapine stopped in
1976."
But
"Clozapine reemerged in 1988. Unlike
the 'typical' anti-psychotics, it does not appear to cause Tardive Dyskinesia,
and it does not seem to raise Prolactin.
"A long-term risk of Clozapine - and
other anti-psychotics - is the Metabolic Syndrome - from weight gain to diabetes
to cardiovascular damage to premature death.
"The Maudsley Guidelines carry a huge
section (pages 62 to 77) on Clozapine side effects - about which a portion of
psychiatric nurses seem not to be aware."
https://www.bmj.com/content/363/bmj.k5421/rr-5 [4352]
Clearly, taking a pill cannot
objectively make the world less annoying, stop your wife leaving you, increase
your income, or make the weather better. If the harvest fails, or your home is
destroyed in an earthquake, depression is a problem, but what are the options,
since the depressing stimuli cannot simply be magicked away? Isn't depression,
after all, a rather rational and realistic response to overwhelming situations?
Many would argue with the statement
that no consistent biological markers have been found. For instance tumor
necrosis factor alpha is implicated, according to Simen et al at the Department
of Psychiatry, Division of Molecular Psychiatry, Yale University, New Haven,
Connecticut, who:
"...show that deletion of either
TNFR1 or TNFR2 leads to an antidepressant-like response in the forced swim test
and that mice lacking TNFR2 demonstrate a hedonic response in a sucrose drinking
test compared with wildtype littermates. In addition, deletion of TNFR1 leads to
decreased fear conditioning. There were no differences in behavior in anxiety
tests for either null mutant."
They conclude:
"These results are consistent with
the hypothesis that TNFα can induce depression-like symptoms even in the absence
of malaise and demonstrate that both receptor subtypes can be involved in this
response."
https://www.sciencedirect.com/science/article/abs/pii/S000632230501366
[1569]
While at the School of Life Sciences
at the University of Minho in Portugal IL-10 was found to improve the mood of
female mice.
https://repositorium.sdum.uminho.pt/bitstream/1822/8631/1/Mesquita%20JPR.pdf
[1568]
The depressed person could be told to
pull his or her socks up. They can be hosed down with cold water, given ECT, or
have psychosurgery. These became indistinguishable from abuse. Or if they are
rich enough and want their emotions to be taken seriously, patients might
receive a talking cure or spend time in a sanitorium. None of this, for either
reputational or practical or economic reasons, could really compete with the
drug-centred model and so psychiatry became increasingly confined to the
drug-centred model.
For there to be a
psychopharmacological treatment there had to be biochemical mechanisms. But
these were slow in coming, and not long after SSRIs arrived, the chemical
imbalance theory of their action has become increasingly dubious.
Says Gotzsche:
"In 2003, the huge deception became
too much for six psychiatric survivors. They were so angry about the stories
they had been told by their psychiatrists that they sent a letter to the
American Psychiatric Association and other organisations stating that they would
begin a hunger strike unless scientifically valid evidence was provided that the
stories the public had been told about mental disorders were true. They asked
for evidence that major mental illnesses are biologically-based brain diseases
and that any psychiatric drug can correct a chemical imbalance. They also
required the organisations to publicly admit if they were unable to provide such
evidence.
"The medical director of the American
Psychiatric Association tried to get off the hook by saying that, 'The answers
to your questions are widely available in the scientific literature.' In his
book, The art of always being right, philosopher Arthur Schopenhauer calls this
deplorable trick 'Postulate what has to be proven.'
"The hunger strike ended when people
started getting health problems, but the Association bluffed. It stated in a
press release that it would not 'be distracted by those who would deny that
serious mental disorders are real medical conditions that can be diagnosed
accurately and treated effectively.'
"Schopenhauer says about this trick:
'If you are being worsted, you can make a diversion - that is, you can suddenly
begin to talk of something else, as though it had a bearing on the matter in
dispute and afforded an argument against your opponent … it is a piece of
impudence if it has nothing to do with the case, and is only brought in by way
of attacking your opponent.'
"This is one of many examples that
psychiatry is more of a religion than a science. Religious leaders couldn’t have
invented a better bluff, if people had required proof that God exists: 'We
priests and cardinals will not be distracted by those who would deny that God
exists and knows about people’s problems and can treat them effectively.'" [3021]
As far as CaPs are concerned, the
propaganda has been the opposite of that applied to psychiatric drugs. They do
not induce physical dependence, but have been legally conflated with drugs which
do.
On the other hand, plausible
mechanisms of action in depression, addiction, OCD and PTSD have been
demonstrated. Cannabis can cheer you up and also help one relax. Mushrooms can
refresh your interface with the world. Taking these drugs can be revelatory and
fun.
Medical psychopharmacology does not
recognise fun as a cure for depression. If you want fun, the law says, you
should drink alcohol. Alcohol is an addiction-forming depressant. Even its most
ardent supporters would not claim they drink because of an alcohol deficiency,
or because it rectifies a chemical imbalance.
At the same time, the existence of an
endocannabinoid deficiency is taboo. But there are more cannabinoid receptors in
the brain than there are for all of the neurotransmitters put together. However
there is no time to teach the ECS in medical schools, their curricula are too
full already.
https://www.leafly.com/news/science-tech/cannabis-endocannabinoid-system-in-medical-school.
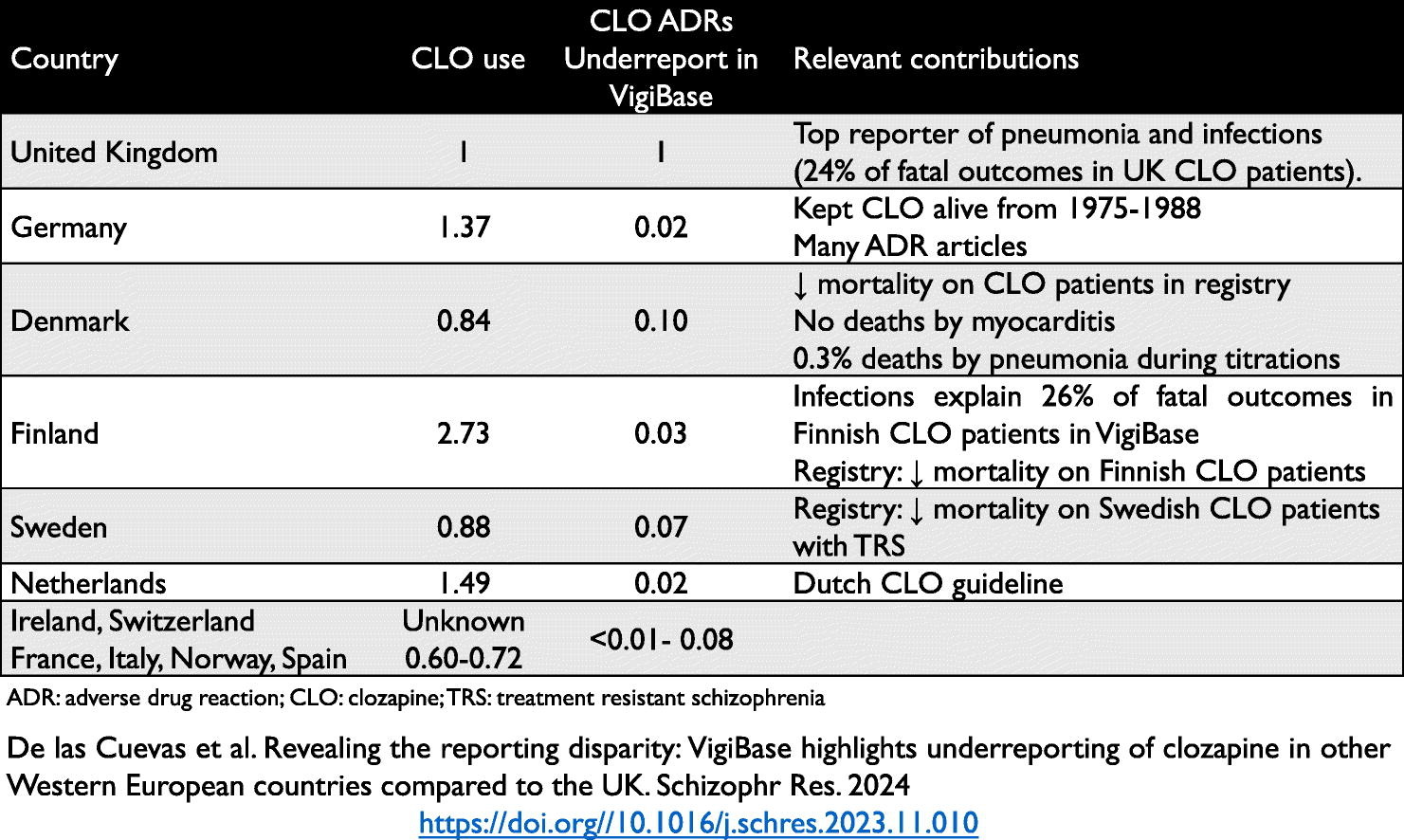
[505]
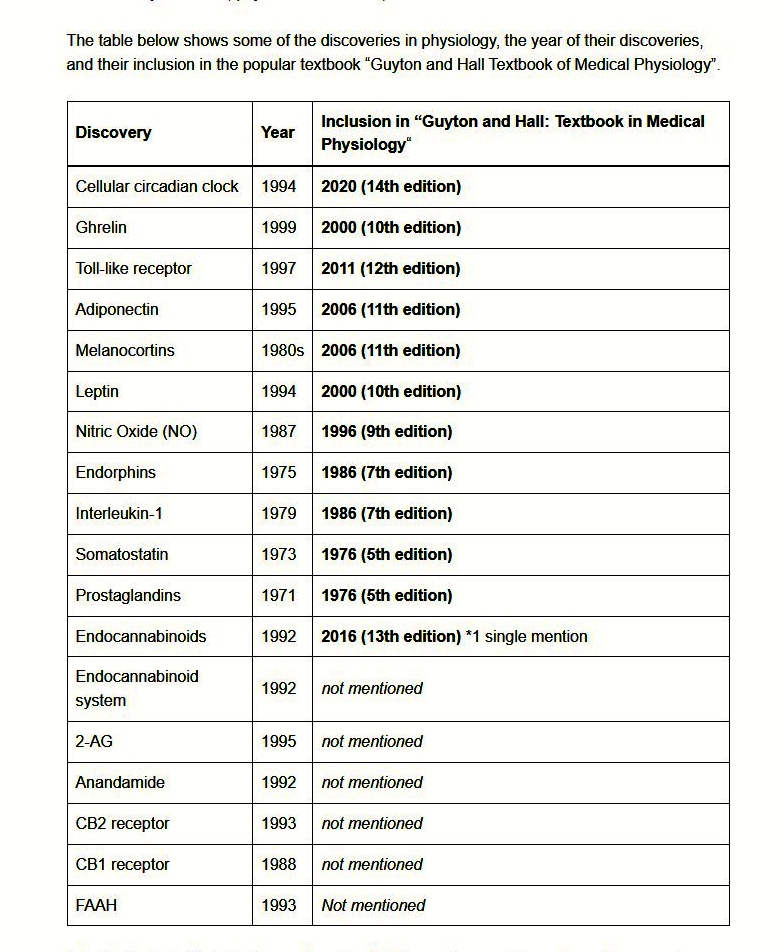
Stefan Broselid, Ph.D.,
Editor-In-Chief of the Aurea Care Science Medical Journal, compared the presence
of ECS-related topics in the popular textbook “Guyton and Hall Textbook of
Medical Physiology”:
"Undoubtedly, the most striking
feature of the table is the complete absence of any mention of the ECS and its
components. The ECS is a biological system composed of endogenous lipid-based
neurotransmitters that bind to cannabinoid receptors in the central and
peripheral nervous system. The ECS is involved in regulating many physiological
and cognitive processes, such as pain, mood, memory, appetite, inflammation, and
immune responses. It also happens to constitute the main pharmacological targets
of the active compounds in cannabis, such as THC and CBD, but this has virtually
nothing to do with its role and importance in human physiology."
And
"In a national survey conducted in
2017, medical school curriculum deans from 101 accredited American medical
schools in the US reported that close to 90% of their residents and fellows do
not feel at all prepared to prescribe medical cannabis and 85% report that they
have received no education at all about the ECS or medical cannabis (Evanoff et
al. 2017)."
The author suggests the name itself
is responsible for the bogeymanisation:
"If it is the unfortunate
nomenclature-based connotation to a misunderstood medical plant that is to
blame, why not change the name of the endocannabinoid system to better reflect
its main functional role rather than its etymological history? After all, if
endocannabinoids had been discovered prior to phytocannabinoids, the ECS quite
likely would have been known for its main function, perhaps as the homeostatic
system? We shouldn’t have to rename it, but I can’t stop thinking about what
would happen."
https://aureamedicalsciencejournal.se/the-missing-chapter-how-human-physiology-textbooks-fail-to-include-the-endocannabinoid-system/
[4861]
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC5648595&blobtype=pdf
[4862]
According to Schroder et al at McLean
Hospital and Harvard Medical School, one problem with a belief in a chemical
imbalance requiring antidepressants is that believing in a chemical imbalance is
depressing:
"We found that although psychosocial
explanations of depression were most popular, biogenetic beliefs, particularly
the belief that depression is caused by a chemical imbalance, were prevalent in
this sample. Further, the chemical imbalance belief related to poorer treatment
expectations. This relationship was moderated by symptoms of depression, with
more depressed individuals showing a stronger relationship between chemical
imbalance beliefs and lower treatment expectations. Finally, the chemical
imbalance belief predicted more depressive symptoms after the treatment program
ended for a 2-week measure of depression (but not for a 24-hour measure of
depression), controlling for psychiatric symptoms at admission, inpatient
hospitalizations, and treatment expectations."
https://www.sciencedirect.com/science/article/abs/pii/S0165032720325064
[4421]
MDMA is very obviously a useful
treatment for PTSD. Serious suicidal ideation (a score of 4 or 5 on the C-SSRS)
was minimal during the study and occurred almost entirely in the placebo arm.
https://www.nature.com/articles/s41591-021-01336-3 [506]
https://cssrs.columbia.edu/wp-content/uploads/C-SSRS_Pediatric-SLC_11.14.16.pdf
[3022]
In all of this, it is of tantamount
importance to psychiatry and the law is that fun and health are not to be
connected. Apparently, the important message to keep front and centre is the one
about depression, not the one about happiness.
The safety of illegal drugs used in
happiness, or amelioration of unwanted states, is not determined by their
legality. They do not become safer when they are decriminalised, or less
effective when outlawed. When, in 1992, the Vatican decided to admit Galileo was
right, the solar system did not abandon a geocentric arrangement and reposition
itself into a new legal format. In the event of future legislative changes, a
return to geocentricism can be guaranteed
Cannabis has been a medicine for
thousands of years
https://link.springer.com/article/10.1007/s12231-016-9351-1 [507] and the
scourge of humanity for a hundred. Psychedelics have played a part in the
development of civilisation, Richard Nixon and the American war effort somewhat
less so.
Suicodologists in Quebec found that
the devil in the weed was in the detail:
In longitudinal cross-lagged
analyses, weekly cannabis use at age 15 was associated with greater odds
(OR=2.19, 95% CI=1.04-4.58) of suicidal ideation two years later. However, other
substance use (alcohol, tobacco, other drugs) fully explained this association.
https://www.sciencedirect.com/science/article/abs/pii/S0165032720309344?via%3Dihub
[508]
This is confirmed by Stern et al
(2025)
"Adolescent sibling groups were recruited from Denver and San Diego (N = 1,261);
at least one sibling was recruited from a substance use treatment program,
alternative school, or juvenile probation. Participants completed clinical
interviews assessing substance use and suicidality at three waves (2001-–2019).
Cannabis use frequency was examined as a predictor of suicidality using
multilevel models accounting for shared familial influences and within-family
clustering. Covariates included alcohol, tobacco, other substance use, age, and
sex. Reverse associations and exploratory models assessing tobacco as a
predictor were also examined.
"Results
Cannabis use was not associated with suicidality (all p’s > 0.05). Exploratory
analyses suggested a possible association between tobacco and suicidality (e.g.,
Wave 1 within-family effect: OR = 1.037, p = 0.016), though these associations
were largely reduced to non-significance after accounting for other substance
use.
"Conclusions
Findings in this high-risk clinical sample are inconsistent with literature
linking cannabis use to suicidality in community samples. Results underscore the
need for further research on the association between general and polysubstance
use risk and suicidality."
https://www.sciencedirect.com/science/article/pii/S2352853225000380 [5826]
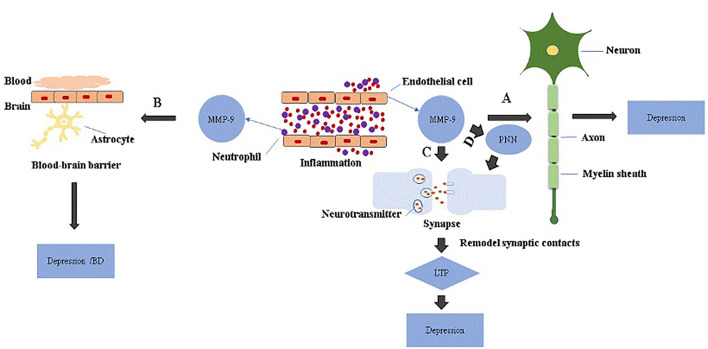
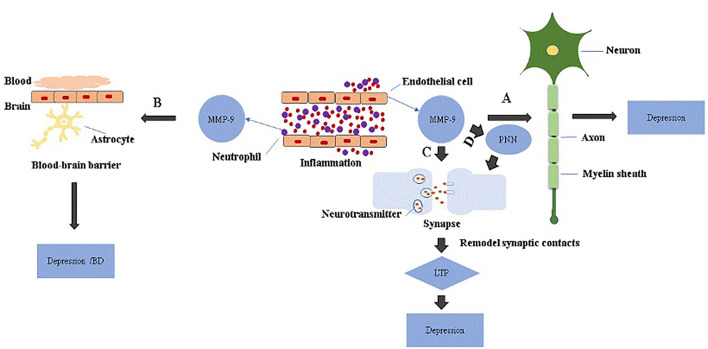
Meanwhile, in "Matrix
Metalloproteinase-9 as an Important Contributor to the Pathophysiology of
Depression" Hongmin Li et al at The Department of Cerebrovascular Diseases, The
Second Affiliated Hospital of Zhengzhou University, Zhengzhou, China
"Among MMP members, the most
important may be MMP−9. It is implicated in the remodeling and stabilization of
dendritic spines, pre and post-synaptic receptor dynamics, consolidation of long
term potentiation, synaptic pruning and myelin formation. MMP-9 is also involved
in the sprouting, pathfinding and regeneration of axons."
As for depression:
"The role of MMP-9 in the pathology
of depression. MMP-9 is elevated in endothelial cells and neutrophils during
inflammation. (A) Excessive MMP-9 is thought to be involved in demyelination
associated with depression. (B) MMP-9 disrupts BBB through tight junction
proteins or basement membrane degradation, which increases neuroinflammation and
may be linked to depression or bipolar disorders with cognitive decline. (C)
Activated MMP-9 localizes in part to synapses and is involved in synaptic
pruning essential for longterm potentiation (LTP), and attenuation of cortical
synaptic LTP-like plasticity; collectively, these are thought to contribute to
depression. (D) MMP-9 remodels perineuronal nets that participate in synaptic
stabilization and limit synaptic plasticity. Depression may occur when
perineuronal net signaling is aberrant."
"Domenici et al. reported that MMP-9
in serum was significantly higher in patients with major depressive disorders (n
= 245) vs. controls. Rybakowski et al. performed a study on 54 in-patients with
bipolar mood disorder and 29 control subjects. An increase of serum MMP-9 at the
early stages of bipolar illness is found to accompany only the depressive
episodes and not manic ones."
Among the human highlights
"Alaiyed et al. reported that MMP-9
levels were elevated in prefrontal cortex of antidepressant-treated patients
with major depressive disorders."
and
"MMP-9 inhibitors possess potential
therapeutic effects for depression."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8971905 [1640]
"As bipolar disorder and marijuana
use are individually associated with cognitive impairment, it also remains
unclear whether there is an additive effect on cognition when bipolar patients
use marijuana. The current study aimed to determine the impact of marijuana on
mood in bipolar patients and to examine whether marijuana confers an additional
negative impact on cognitive function. Twelve patients with bipolar disorder who
smoke marijuana (MJBP), 18 bipolar patients who do not smoke (BP), 23 marijuana
smokers without other Axis 1 pathology (MJ), and 21 healthy controls (HC)
completed a neuropsychological battery. Further, using ecological momentary
assessment, participants rated their mood three times daily as well as after
each instance of marijuana use over a four-week period. Results revealed that
although the MJ, BP, and MJBP groups each exhibited some degree of cognitive
impairment relative to HCs, no significant differences between the BP and MJBP
groups were apparent, providing no evidence of an additive negative impact of
BPD and MJ use on cognition. Additionally, ecological momentary assessment
analyses indicated alleviation of mood symptoms in the MJBP group after
marijuana use; MJBP participants experienced a substantial decrease in a
composite measure of mood symptoms. Findings suggest that for some bipolar
patients, marijuana may result in partial alleviation of clinical symptoms.
Moreover, this improvement is not at the expense of additional cognitive
impairment."
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0157060
[2448]
In astonishing news, science has now
discovered that cannabis makes you happy, describing this in the Yale Journal of
Biological Medicine (2020) as a "positive side effect".
Li et al (2020) examined "The
Effectiveness of Cannabis Flower for Immediate Relief from Symptoms of
Depression":
"We observed 1,819 people who
completed 5,876 cannabis self-administration sessions using the ReleafApp™
between 06/07/2016 and 07/08/2019, with the goal of measuring real-time effects
of consuming Cannabis flower for treating symptoms of depression. Results: On
average, 95.8% of users experienced symptom relief following consumption with an
average symptom intensity reduction of –3.76 points on a 0-10 visual analogue
scale (SD = 2.64, d = 1.71, p <.001). Symptom relief did not differ by labeled
plant phenotypes (“C. indica,” “C. sativa,” or “hybrid”) or combustion method.
Across cannabinoid levels, tetrahydrocannabinol (THC) levels were the strongest
independent predictors of symptom relief, while cannabidiol (CBD) levels,
instead, were generally unrelated to real-time changes in symptom intensity
levels. Cannabis use was associated with some negative side effects that
correspond to increased depression (e.g. feeling unmotivated) in up to 20% of
users, as well as positive side effects that correspond to decreased depression
(e.g. feeling happy, optimistic, peaceful, or relaxed) in up to 64% of users.
Conclusions: The findings suggest that, at least in the short term, the vast
majority of patients that use cannabis experience antidepressant effects,
although the magnitude of the effect and extent of side effect experiences vary
with chemotypic properties of the plant."
and
"One of the most clinically relevant
findings from this study was the widely experienced relief from depression
within 2 hours or less. Because traditional antidepressants have times-to-effect
in weeks, short-term Cannabis use might be a solution to these delays in
treatment or could be used to treat acute episodes associated with suicidal
behavior and other forms of violence."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7309674/ [2447]
In 2024, Specka et al made the same
discovery again, in a retrospective longitudinal 18 week study of 59 outpatients
with MDD who had previously tried antidepressants - in "Effectiveness of Medical
Cannabis for the Treatment of Depression: A Naturalistic Outpatient Study":
"Patients were 20-54 years old; 72.9%
were male; one third reported times of regular cannabis consumption within the
previous five years. Drop-out rate was 22% after 18 weeks. Mean severity of
depression decreased from 6.9 points (SD 1.5) at entry to 3.8 points (2.7) at
week 18 (baseline observation carried forward; 95% CI for the mean difference:
2.4 to 3.8; p<0.001). A treatment response (>50% reduction of the initial score)
was seen in 50.8% at week 18. One third of patients complained about side
effects, none was considered as severe. Concomitant antidepressant medication
(31% of patients) was not associated with outcome."
https://pubmed.ncbi.nlm.nih.gov/38211630/ [4366]
And in fact this discovery reoccurs
every now and then. In 2009 the Laboratory of Neuroendocrinology, The
Rockefeller University, New York researchers Hill et al considered "The
therapeutic potential of the endocannabinoid system for the development of a
novel class of antidepressants", stating:
"Substantial evidence has accumulated implicating a deficit in endocannabinoid
in the etiology of depression; accordingly, pharmacological augmentation of
endocannabinoid signaling could be a novel target for the pharmacotherapy of
depression. Within preclinical models, facilitation of endocannabinoid
neurotransmission evokes both antidepressant and anxiolytic effects. Similar to
the actions of conventional antidepressants, enhancement of endocannabinoid
signaling can enhance serotonergic and noradrenergic transmission; increase
cellular plasticity and neurotrophin expression within the hippocampus; and
dampen activity within the neuroendocrine stress axis. Furthermore, limbic
endocannabinoid activity is increased by both pharmacological and somatic
treatments for depression, and, in turn, appears to contribute to some of the
neuroadaptive alterations elicited by these treatments. These preclinical
findings support the rationale for the clinical development of agents which
inhibit the cellular uptake and/or metabolism of endocannabinoids in the
treatment of mood disorders."
https://pubmed.ncbi.nlm.nih.gov/19732971/ [4385]
We await those clinical agents with some skepticism and trepidation and we'll
just be ok with weed, thanks.
In a 2023-published longitudinal
comparison of mortality rates in bipolar disorder with common causes of
mortality Yocum et al at the University of Michigan began by examining deaths
and associated variables among 1,128 participants who had volunteered for the
program's long-term study of individuals with and without bipolar disorder."
They discovered that the 847 study
participants with bipolar disorder accounted for all but two of the 56
fatalities that have occurred since the study's start in 2006. Their analysis,
adjusting for statistical differences, reveals that a person with a diagnosis of
bipolar disorder was six times more likely to die over a 10-year period than
participants in the same study without a bipolar disorder diagnosis.
To see if they could discover the
same effect, the researchers then looked to another data source. More than
18,000 patients who receive primary care from Michigan Medicine, the academic
medical centre at the University of Michigan, had years' worth of anonymous
patient records examined by the researchers. Those in this group who had a
history of bipolar disorder had a four-fold higher risk of passing away during
the study period than those who did not.
High blood pressure was the only
factor in this group of individuals linked to an even higher risk of passing
away during the study period. Regardless of bipolar disorder, the risk of death
was five times higher for those with hypertension than for those with normal
blood pressure. In contrast, regardless of bipolar status, smokers were twice as
likely to die in this sample as never-smokers, and those over 60 were three
times more likely to die. McInnis, a psychiatry professor at the University of
Michigan Medical School, stated, "To our major surprise, in both samples we
found that having bipolar disorder is far more of a risk for premature death
than smoking."
https://economictimes.indiatimes.com/industry/healthcare/biotech/healthcare/bipolar-disorder-can-make-you-die-early-says-study-key-findings/bipolar-disorder-and-death/slideshow/106638965.cms
[4323]
https://www.sciencedirect.com/science/article/abs/pii/S0165178123005516?via%3Dihub
[4324]
It is fairly simple - the Defence
hopes not simplistic - to infer that the benefits reported in [2448]
will ameliorate the tendency to die reported in [4324]
via positive effects on both mood and cardiometabolic stress.
Those seeking a more convenient route
through the system could go to the pub, where they will at the very least lose
some dignity, and at worst kill somebody.
Alternatively they could go and get
some cannabis, which according to Li et al [2447]
works immediately, altering their perception of the situation by raising their
hedonic tone.
But if you insist on banning the one
thing that will help without anyone getting their face smashed in, and if you
insist on banning something which is impossible to ban - so drunk people in Ptuj
can pick and choose enemies upon whom they can unleash their rage - ban
depressed people. Not cannabis and psychedelics.
In 2022, Miranda et al found cannabis
had "uniquely beneficial effects" in bipolar patients:
"Cannabis use is highly prevalent in
people with bipolar disorder (BD), with many reporting using cannabis to
ameliorate symptoms. These symptoms include deficits in goal-directed behaviors
(i.e., decision-making and hyper-motivation) and cognitive function (i.e.,
attention and learning). However, chronic cannabis use is also associated with
cognitive impairment, thus it is unclear to what degree cannabis is useful in
ameliorating symptoms of BD. Here, we determined the effects of chronic cannabis
use on goal-directed behavior and cognition that are impaired in people with BD.
We recruited BD+ and BD- participants that were either cannabis users (C+) or
non-users (C-). We performed a 2X2 ANOVA on interim data using BD and cannabis
use as between-subjects factors on the 4 diagnostic groups: BD-/C- (n=25),
BD-/C+(n-21), BD+/C- (n=8) and BD+/C+ (n=12). Participants were tested with a
cognitive battery measuring risky decision-making (Iowa Gambling Task; IGT),
motivation (Progressive Ratio Breakpoint Ratio Task; PRBT), reward learning
(Probabilistic Learning Task; PLT) and sustained attention (5-C CPT). Overall,
cannabis users were younger than non-users. Using age as a covariate, we
observed BD x cannabis interaction effects on the IGT and PRBT. BD+/C+
participants showed less risk-prone behaviors on the IGT (F (1,63), p=.015,
ES=.09) and normalized motivation on the PRBT (F (1,61), p=.045, ES=.065). We
observed moderate effects of cannabis on punishment sensitivity (F (1,63),
p=0.059, ES=0.055) and sustained attention (F (1,48), p=0.056, ES=0.074).
Chronic cannabis use was associated with a modest improvement in some cognitive
functions. Cannabis use was also associated with a normalization of risky
decision making and effortful motivation in people with BD, but not healthy
participants. Thus, chronic cannabis use may have uniquely beneficial effects in
people with BD. Previous studies suggest that some people with BD have increased
dopaminergic activity due to a reduced dopamine transporter expression. Chronic
cannabis use has been shown to reduce dopamine release, thus chronic cannabis
use may result in a return to dopamine homeostasis in people with BD and
consequently normalizing their deficits in goal directed behaviors. We are
engaged in additional studies that explore this potential
dopaminergic/endocannabinoid mechanism."
https://www.abstractsonline.com/pp8/#!/10619/presentation/84925 [2445]
"To pin down the effects of cannabis
on those with bipolar, researchers recruited people with and without the
disorder, along with cannabis users and non-users in each group, analyzing each
combination. Participants were tested on cognitive battery measuring risky
decision-making, reward-learning, and sustained attention.
"Ultimately, researchers confirmed
that cannabis indeed could hold some special benefits for those with bipolar,
specifically in helping to reduce risky decision-making. Researchers also
suggested that cannabis reduces the dopaminergic activity in the brain, which
helps suppress symptoms, and found that cannabis had moderate effects on
punishment sensitivity and sustained attention.
According to Colizzi et al (2019):
"'Chronic cannabis use was associated
with a modest improvement in some cognitive functions,' authors noted. 'Cannabis
use was also associated with a normalization of risky decision making and
effortful motivation in people with [bipolar disorder], but not healthy
participants. Thus, chronic cannabis use may have uniquely beneficial effects in
people with [bipolar disorder].'"
https://hightimes.com/health/study-cannabis-has-uniquely-beneficial-effects-on-people-with-bipolar-disorder/
[2446]
This aligns with the metabolic
overdrive hypothesis of bipolar: hyperglycolysis and
glutaminolysis in bipolar mania.
According to Campbell and Campbell (2024):
"Evidence from diverse areas of
research including chronobiology, metabolomics and magnetic resonance
spectroscopy indicate that energy dysregulation is a central feature of bipolar
disorder pathophysiology. In this paper, we propose that mania represents a
condition of heightened cerebral energy metabolism facilitated by
hyperglycolysis and glutaminolysis. When oxidative glucose metabolism becomes
impaired in the brain, neurons can utilize glutamate as an alternative substrate
to generate energy through oxidative phosphorylation. Glycolysis in astrocytes
fuels the formation of denovo glutamate, which can be used as a mitochondrial
fuel source in neurons via transamination to alpha-ketoglutarate and subsequent
reductive carboxylation to replenish tricarboxylic acid cycle intermediates.
Upregulation of glycolysis and glutaminolysis in this manner causes the brain to
enter a state of heightened metabolism and excitatory activity which we propose
to underlie the subjective experience of mania. Under normal conditions, this
mechanism serves an adaptive function to transiently upregulate brain metabolism
in response to acute energy demand. However, when recruited in the long term to
counteract impaired oxidative metabolism it may become a pathological process."
https://www.openread.academy/en/paper/reading?corpusId=50309855 [4761]
"A limited number of studies
consistently support the evidence for altered brain glutamate levels as measured
by proton magnetic resonance spectroscopy (1H-MRS) in otherwise healthy chronic
cannabis users, with all but one of the five studies indicating reduced levels
of glutamate-derived metabolites Glutamate (Glu) or Glutamate + Glutamine (Glx)
in both cortical and subcortical brain areas."
https://www.nature.com/articles/s41380-019-0374-8 [4760]
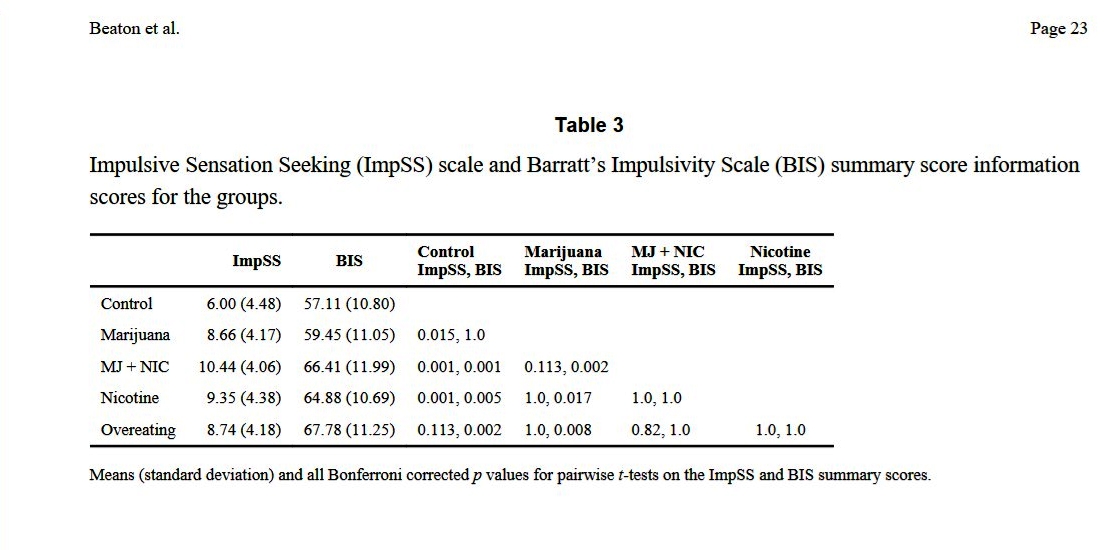
In a sample of 297 with a mean age
below 30, Beaton et al (2016) found the illegal weed users were more sensible
than the legal nicotine addicts:
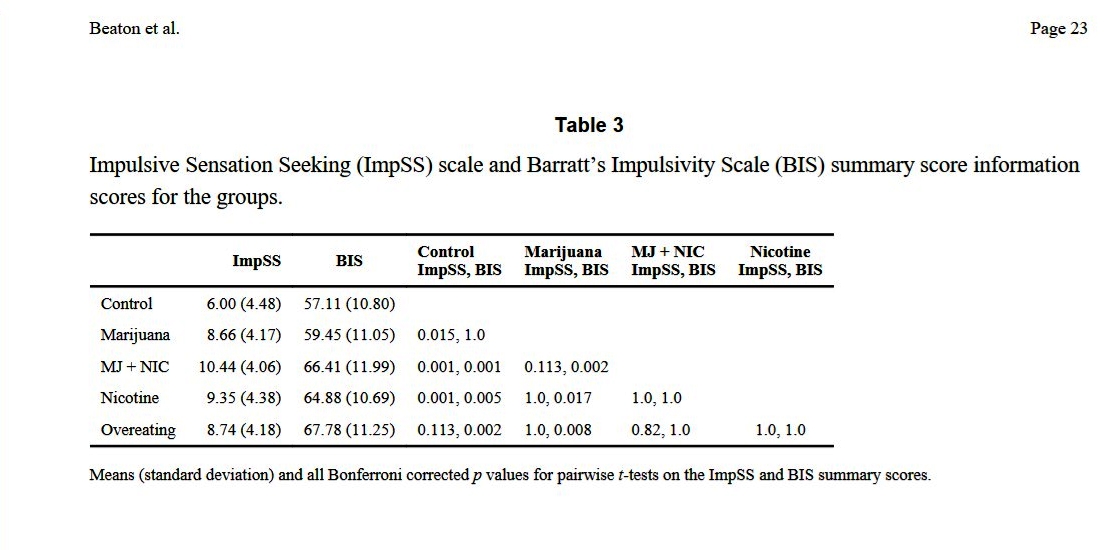
"Post-hoc comparisons showed that the
Control and Marijuana groups were less impulsive than the Marijuana+Nicotine,
Nicotine, and Overeating groups (Table 3)."
"Impulsive Sensation Seeking (ImpSS)
and Barratt's Impulsivity scales (BIS) Scales were analyzed with a
non-parametric factor analytic technique (discriminant correspondence analysis)
to identify group-specific traits on 297 individuals from five groups: Marijuana
(n = 88), Nicotine (n = 82), Overeaters (n = 27), Marijuauna + Nicotine (n =
63), and CONTROLs (n = 37).
"Results: A significant overall
factor structure revealed three components of impulsivity that explained
respectively 50.19% (pperm < 0.0005), 24.18% (pperm < 0.0005), and 15.98% (pperm
< 0.0005) of the variance. All groups were significantly different from one
another. When analyzed together, the BIS and ImpSS produce a multi-factorial
structure that identified the impulsivity traits specific to these groups. The
group specific traits are (1) CONTROL: low impulse, avoids thrill-seeking
behaviors; (2) Marijuana: seeks mild sensation, is focused and attentive; (3)
Marijuana + Nicotine: pursues thrill-seeking, lacks focus and attention; (4)
Nicotine: lacks focus and planning; (5) Overeating: lacks focus, but plans
(short and long term).
"Conclusions: Our results reveal
impulsivity traits specific to each group."
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC4318510&blobtype=pdf
[3922]
In similar attention to the same
detail, Round et al (2020) found:
"Trait impulsivity was significantly
higher in cigarette smokers than non-smokers, irrespective of cannabis use,
except for motor impulsivity, where cigarette smoking was only associated with
elevated trait impulsivity in non-smokers of cannabis. Dimensions of trait
impulsivity were significantly positively related to cigarette smoking frequency
and nicotine dependence, but not to cannabis smoking frequency or dependence.
Smoking cigarettes or cannabis was associated with significantly impaired
reflection impulsivity relative to not smoking either substance. However, no
additional increases in reflection impulsivity were observed in those who smoked
both cigarettes and cannabis. No group differences in response inhibition were
detected."
Trait impulsivity in detail:
"There were significant main effects
for cigarette smoking status on BIS-11 total scores (F(1, 220) = 32.76, p <
.001, ηp 2 = .13), along with the attention (F(1, 220) = 15.63, p < .001, ηp 2 =
.07) and non-planning subscales (F(1, 220) = 27.95, p < .001, ηp 2 = .11), such
that individuals who smoked cigarettes scored significantly higher than those
who did not smoke cigarettes (Figure 1(a) to (c)). No significant effects of
cannabis smoking or interactions were found (all F(1, 220) < 2.27, p ⩾ .101, ηp
2 ⩽ .01). For the BIS-11 motor impulsivity subscale, there was again no
significant main effect of cannabis (F < 1, p = .773, ηp 2 < .001), but a
significant main effect of cigarette smoking (F(1, 220) = 19.14, p < .001, ηp 2
= .08), this time qualified by a significant cigarette smoking × cannabis
smoking interaction (F(1, 220) = 5.92, p = .016, ηp 2 = .03; see Figure 1d).
Cigarette smoking was again associated with higher levels of impulsivity, but
simple effects analyses showed that this effect was seen in NS (p<.001), but not
smokers (p = .178) of cannabis. Motor impulsivity did not differ as a function
of cannabis smoking in either cigarette smokers (p = .095) or non-cigarette
smokers (p=.078)."
https://journals.sagepub.com/doi/pdf/10.1177/0269881120926674?download=true
[3923]
"A Naturalistic Examination of the
Acute Effects of High-Potency Cannabis on Emotion Regulation Among Young Adults:
A Pilot Study" by Cavalli et al (2024) made the horrifying finding that:
"Participants reported a more
positive mood and decreases in anxiety while intoxicated. There was no evidence
that acute high-potency cannabis affected participants' implicit or explicit
emotion regulation task performance."
https://onlinelibrary.wiley.com/doi/10.1002/hup.2915 [5194]
"Potentiation of GABA by either CBD
or 2-AG is selective for the α2 subunit" report Bakas et al (2017).
https://www.sciencedirect.com/science/article/abs/pii/S1043661816311392?via%3Dihub
[3926]
Adolescent cannabis users showed
lower GABA in a small study of just 39 subjects by Subramaniam et al in Salt
Lake City, where sales of tea and coffee are presumably quite low. But:
"Assessment of impulsive behavior
demonstrated no significant between-group differences in motor, non-planning,
attention, and total impulsivity scores. Additionally, impulsivity measures and
tissue-corrected GABA+ or Glx levels were not significantly correlated in either
group."
https://www.sciencedirect.com/science/article/abs/pii/S03768716220006317
[3927]
The University of Utah is not
affiliated with the LDS, but Mormon attendance is reckoned at 25-50%. Given this
venue, it may be that the Mormons are increasing their impulsivity and denying
themselves a good night's sleep. Tea accumulates GABA and a special process has
been devised to produce high-GABA tea.
https://en.wikipedia.org/wiki/GABA_tea [3924]
Although there has been a debate
about whether oral GABA can even cross the blood-brain barrier, collected
studies using tea, coffee, rice and other dietary sources, a review by Hepsomali
et al (2020) - based in various non-Mormon places from Nottingham to Hokkaido -
found mildly convincing evidence for benefits upon stress and sleep.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7527439/ [3925]
Cannabis is not the only influence on
GABA. The Defendant wonders on what superstitious or empirical basis cannabis
could be held responsible for legal transgressions when alcohol would not.
Compass Pathways plc published some
results on psychedelics and depression in 2021:
"In the randomised, controlled,
double-blind trial, a single dose of investigational COMP360 psilocybin was
given to 233 patients in conjunction with psychological support from specially
trained therapists. All patients discontinued antidepressants prior to
participation. The trial was powered to compare two active doses of COMP360,
25mg and 10mg, against a comparator 1mg dose. The 25mg group vs the 1mg group
showed a -6.6 difference on the MADRS* depression scale at week 3 (p<0.001). The
25mg group demonstrated statistical significance on the MADRS efficacy endpoint
on the day after the COMP360 psilocybin administration (p=0.002). The 10mg vs
1mg dose did not show a statistically significant difference at week 3. The
MADRS was assessed by independent raters who were remote from the trial site,
and blind to intervention and study design, effectively creating a triple blind.
"At least twice the number of
patients in the 25mg group showed response and remission* at week 3 and week 12,
compared with the 1mg group. The protocol-defined sustained response* up to week
12 was double, with 20.3% of patients in the 25mg group vs 10.1% in the 1mg
group. Using a definition of sustained response* that is consistent with other
TRD studies, the difference was more than double, with 24.1% of patients in the
25mg group vs 10.1% in the 1mg group."
https://ir.compasspathways.com/news-releases/news-release-details/compass-pathways-announces-positive-topline-results
[4310]
Another report that year by
Carhart-Harris et al compared psilocybin and escitalopram. Psilocybin worked
better. The subjects were tested using the 16-item Quick Inventory of Depressive
Symptomatology–Self-Report (QIDS-SR-16; scores range from 0 to 27, with higher
scores indicating greater depression.
"A total of 59 patients were
enrolled; 30 were assigned to the psilocybin group and 29 to the escitalopram
group. The mean scores on the QIDS-SR-16 at baseline were 14.5 in the psilocybin
group and 16.4 in the escitalopram group. The mean (±SE) changes in the scores
from baseline to week 6 were −8.0±1.0 points in the psilocybin group and
−6.0±1.0 in the escitalopram group, for a between-group difference of 2.0 points
(95% confidence interval [CI], −5.0 to 0.9) (P=0.17). A QIDS-SR-16 response
occurred in 70% of the patients in the psilocybin group and in 48% of those in
the escitalopram group, for a between-group difference of 22 percentage points
(95% CI, −3 to 48); QIDS-SR-16 remission occurred in 57% and 28%, respectively,
for a between-group difference of 28 percentage points (95% CI, 2 to 54). Other
secondary outcomes generally favored psilocybin over escitalopram, but the
analyses were not corrected for multiple comparisons. The incidence of adverse
events was similar in the trial groups."
https://www.nejm.org/doi/full/10.1056/NEJMoa2032994 [4311]
"The Montgomery–Åsberg Depression
Rating Scale (MADRS) is a ten-item diagnostic questionnaire which psychiatrists
use to measure the severity of depressive episodes in patients with mood
disorders. It was designed in 1979 by British and Swedish researchers (Marie
Åsberg) as an adjunct to the Hamilton Rating Scale for Depression (HAMD) which
would be more sensitive to the changes brought on by antidepressants and other
forms of treatment than the Hamilton Scale was. There is, however, a high degree
of statistical correlation between scores on the two measures.
and
"The questionnaire includes questions
on ten symptoms:
"Apparent sadness
Reported sadness
Inner tension
Reduced sleep
Reduced appetite
Concentration difficulties
Lassitude
Inability to feel
Pessimistic thoughts
Suicidal thoughts
"Each item yields a score of 0 to 6;
the overall score thus ranges from 0 to 60. Higher MADRS score indicates more
severe depression. Usual cutoff points are:
"0 to 6: normal/symptom absent
7 to 19: mild depression
20 to 34: moderate depression
35 to 60: severe depression."
https://en.wikipedia.org/wiki/Montgomery%E2%80%93%C3%85sberg_Depression_Rating_Scale
[4257]
In 2021 Aaronson et al embarked upon
"Single-Dose Synthetic Psilocybin With Psychotherapy for Treatment-Resistant
Bipolar Type II Major Depressive Episodes. A Nonrandomized Controlled Trial"
(2023)...
"Bipolar II disorder (BDII) is a
lifelong condition characterized by recurrent hypomanic and depressive episodes
with a lifetime prevalence of at least 0.4% among adults. It causes a level of
functional impairment and disability comparable to bipolar I disorder (BDI)
Despite treatment, patients with BDII are typically symptomaticmost of the time,
primarily experiencing protracted and difficult-to-treat periods of depression.
Bipolar disorder has high mortality, as 30% of affected individuals attempt and
5% to 15% commit suicide. Historically, BDII was viewed as the lesser of the
bipolar disorders due to the absence of florid mania. However, recent studies
document that functional impact and risk of suicide are similar in BDI and
BDII."
and
"INTERVENTIONS A single dose of
synthetic psilocybin, 25 mg, was administered. Psychotropic medications were
discontinued at least 2 weeks prior to dosing. Therapists met with patients for
3 sessions during pretreatment, during the 8-hour dosing day, and for 3
integration sessions posttreatment.
"MAIN OUTCOMES AND MEASURES The
primary outcome measure was change in Montgomery-Åsberg Depression Rating scale
(MADRS) at 3 weeks posttreatment. Secondary measures included MADRS scores 12
weeks posttreatment, the self-rated Quick Inventory of Depression Symptoms-Self
Rating (QIDS-SR), and the self-rated Quality of Life Enjoyment and Satisfaction
Questionnaire-Short Form (Q-LES-Q-SF), each completed at baseline and all
subsequent visits. Safety measures included the Columbia Suicide Severity Rating
Scale (CSSRS) and the Young Mania Rating Scale (YMRS) completed at each visit.
"RESULTS Of the 15 participants in
this study (6 male and 9 female; mean [SD] age, 37.8 [11.6] years), all had
lower scores at week 3, with a mean (SD) change of −24.00 (9.23) points on the
MADRS, (Cohen d = 4.08; 95% CI, −29.11 to −18.89; P < .001). Repeat measures
analysis of variance showed lower MADRS scores at all tested posttreatment time
points, including the end point (Cohen d = 3.39; 95% CI, −33.19 to −16.95;
adjusted P < .001). At week 3, 12 participants met the response criterion (50%
decrease in MADRS), and 11 met remission criterion (MADRS score 10). At the
study end point, 12 patients met both response and remission criteria. QIDS-SR
scores and Q-LES-Q-SF scores demonstrated similar improvements. YMRS and CSSRS
scores did not change significantly at posttreatment compared to baseline."
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2812443 [4256]
In "Psilocybin use in
bipolar disorder: A comprehensive review" Do et al (2026) say:
"Two small clinical trials show that psilocybin
combined with psychotherapy was safe and effective for the treatment of BDII
depression with large treatment effects. No serious adverse events, including
treatment-emergent mania/hypomania or increased suicidality, were reported in
both trials. However, other studies have raised concerns about the safety of
psilocybin in BD patients, including the development or worsening of manic
symptoms, sleep disruptions and anxiety. Overall, the majority of BD patients
believe that psilocybin could benefit their mental health problems, but their
experiences varied depending on several contextual factors, such as
polysubstance use, psilocybin dose, solo versus social experiences and
pre-psilocybin sleep deprivation."
https://www.sciencedirect.com/science/article/pii/S0165032725019275 [5548]
The psychopharmaceutical upheaval continued in 2023
with a reanalysis of the data that made Prozac great.
"Back in 2003, the NIMH-sponsored
Treatment for Adolescents with Depression Study (TADS) included 439 adolescents
aged 12-17 who met DSM-IV criteria for depression. There were four treatment
arms, including fluoxetine (Prozac) only; cognitive-behavioral therapy (CBT)
only; fluoxetine and CBT; and placebo. The psychotherapy groups were not able to
be blinded. The randomized trial lasted for 12 weeks, and participants were
asked which group they believed they were in at both 6 weeks and 12 weeks.
Improvement in depression was measured with the Children’s Depression Rating
Scale–Revised (CDRS-R).
"The TADS study is commonly cited as
evidence for Prozac’s effectiveness in depression treatment, because the
combined drug and CBT group did slightly better than the placebo group. However,
the drug group alone did no better than the placebo group in the TADS analysis
of the CDRS-R.
"The current analysis was conducted
as part of the Restoring Invisible and Abandoned Trials (RIAT) initiative, which
allowed the researchers access to the raw data from the TADS study. They
obtained information on the fluoxetine group (109 participants) and the placebo
group (111 participants), since those were the two blinded groups, in order to
directly compare the effects of unblinding.
"In all the groups, more than 60% of
the participants and raters correctly guessed whether they received the drug or
placebo (a perfectly blinded study would result in 50% guessing correctly).
"The researchers found that the
placebo effect was stronger than the actual treatment itself. Those who guessed
that they received the treatment were more likely to improve than those who
guessed they received the placebo—even if their guess was incorrect. That is, on
average, those who believed they received the drug improved, even if they
actually received the placebo. Likewise, those who believed they received the
placebo were less likely to improve, even if they actually received the drug.
"Those who believed they received the
drug, on average, improved by 10 points more on the CDRS-R than those who
believed they received the placebo. Those who believed they received the drug
improved by 26.98 points, on average. Those who believed they received the
placebo improved by 16.65 points, on average.
"Amazingly, the group that did the
best was those who believed they received the drug, but actually received the
placebo. These patients did better than those who received the drug and knew it!
"'Adolescents who guessed they were
on fluoxetine, but were actually allocated to placebo, demonstrated the largest
improvement in CDRS-R,' the researchers write.
"Finally, the researchers confirmed
the initial finding of TADS: after accounting for the placebo effect (treatment
guess), the researchers found that taking Prozac did not improve depression.
"The researchers write, 'Treatment
guess had a substantial and statistically significant effect on outcome
(Children’s Depression Rating Scale-Revised change mean difference 9.12, p <
0.001), but actual treatment arm did not (1.53, p = 0.489).'
"The researchers conclude that
unblinding, which amplifies the placebo effect, may be the reason
antidepressants typically beat placebo by a slight margin in clinical trials.
They add that future studies need to make sure to assess unblinding in order to
provide accurate data on drug efficacy.
"'Our analysis suggests that the
effects that are demonstrated in placebo-controlled trials of antidepressants
may represent amplified placebo effects that are a result of the differential
distribution of expectancy effects caused by unblinding. Since the expectancy
effects are substantial, even a small degree of unblinding might produce an
apparent difference between an active drug and a placebo. For future research,
there is a clear need for more stringent study designs that systematically
record and analyse treatment guesses and assess blindness, and do so early on
and repeatedly,' they write.
"Moreover, since clinical practice
guidelines are based on evidence from studies like TADS, the researchers argue
that guideline authors need to reassess the evidence base for their
recommendations. Recommending antidepressants on the basis of studies like TADS
is poor science."
https://www.madinamerica.com/2023/12/placebo-effect-not-antidepressants-responsible-for-depression-improvement/
[4297]
From tests in mice, Themann et al
(2025) feel "Prozac exposure during adolescence increases pain sensitivity in
adulthood":
"Preclinical work indicates that
early-life exposure to FLX alters neurobehavioral responses as a function of age
(Kryst et al., 2022; Olivier et al., 2011). For example, adult rodents with
juvenile FLX pre-exposure display increases in anxiety-related behavior
(Flores-Ramirez et al., 2021; Iñiguez et al., 2010), altered responses to
inescapable stress (Iñiguez et al., 2010; Karpova et al., 2009), impaired
spatial memory performance (Flores-Ramirez et al., 2019) and changed preference
to commonly abused drugs, like cocaine (Flores-Ramirez et al., 2018; Iñiguez et
al., 2015; Warren et al., 2011) and nicotine (Alcantara et al., 2014). Such
enduring FLX-induced behavioral changes are accompanied by neurobiological
deviations within multiple brain regions including the hippocampus (Iñiguez et
al., 2021; Kroeze et al., 2015; Sierra-Fonseca et al., 2021), prefrontal cortex
(Themann et al., 2022), ventral tegmental area (Alcantara et al., 2014; Iñiguez
et al., 2014), and amygdala (Homberg et al., 2011) – which comprise key
brain-circuitry known to impact emotion regulation. Consequently, signifying
that early life exposure to FLX, resulting in chronic elevations of serotonin,
may predispose individuals to undesired mood-related symptomatology in
adulthood.
"Antidepressant medications (Coluzzi
and Mattia, 2005; Hache et al., 2011; Trujillo and Iñiguez, 2020), including FLX
(Hache et al., 2012), are able to reverse hyperalgesia in animal models for the
study of nociception. This is not surprising because there is a correlation
between depression symptoms, inflammation, and pain sensitivity (Chan et al.,
2019; Hamdy et al., 2018; Humes et al., 2024; Tesic et al., 2023). Because SSRI
prescriptions are on the rise in the juvenile population, with such treatment
lasting for years, it is possible that adolescent FLX exposure may impact
responses to pain perception in later life (Baudat et al., 2022). Indeed, recent
clinical evidence suggests that adolescent exposure to FLX increases the levels
of the inflammation markers interleukin-6 (IL-6) and interleukin 1-Beta (IL-1β)
six months after treatment (Amitai et al., 2020). For this reason, the goal of
this preclinical investigation is to examine whether chronic FLX exposure during
the juvenile stage of development alters responses to thermal nociception in
adulthood, using female mice as a model system."
And...
"The long-term effects of juvenile
FLX exposure (PD35-49) on HPT behavioral responses in adult (PD70) female
C57BL/6 mice are shown in Fig. 1B. Mean differences in time (s) to lick a
hindpaw were noted as a function of juvenile SSRI pre-exposure (n = 10 per
group). Specifically, adult female mice with FLX history displayed shorter
latency to hindpaw lick when compared to VEH-controls (t18 = 2.22, p = 0.03) – a
murine behavioral response indicative of hyperalgesia..."
https://www.sciencedirect.com/science/article/abs/pii/S0022395625002626?via%3Dihub
[5030]
----------------------------------------------------------------------------
The Englishman stands
for the rights of everyone disadvantaged, discriminated against, persecuted, and
prosecuted on the false or absent bases of prohibition, and also believes the
victims of these officially-sanctioned prejudices have been appallingly treated
and should be pardoned and compensated.
The Englishman requests the return of his CaPs and other rightful property, for
whose distraint Slovenia has proffered no credible excuse or cause.
The Benedictions represent both empirical entities as well as beliefs. Beliefs
which the Defence evidence shows may be reasonably and earnestly held about the
positive benefits of CaPs at the population level, in which the good
overwhelmingly outweighs the bad. Below, the latest version of this dynamic
list.
THE BENEDICTIONS
REFERENCES
TIMELINE OF DRUG LAW v. SCIENCE